Open Thoracoabdominal Aneurysm Repair in a 4-Year-Old with Tuberous Sclerosis
Joseph M. Besho MD; Akiko Tanaka MD, Ph.D.; Anthony L. Estrera, MD
Department of Cardiothoracic and Vascular Surgery, McGovern Medical School at UTHealth, Houston, TX, USA
Case Report

Figure 1 – Magnetic Resonance Angiography demonstrating Extent III Thoracoabdominal Aortic Aneurysm measuring 7.0 cm at the mid-descending thoracic aorta and extending from T8-L3.
The patient is a four-year-old male with a history of tuberous sclerosis, diagnosed at 5 months of age. Physical examination demonstrated café-au-lait spots and subcutaneous tubers of the chest, abdomen and lower back. Magnetic resonance angiography showed a thoracoabdominal aneurysm extending from T8-L3 (Fig. 1), measuring 7.0 cm in its maximum diameter at the abdominal aorta with three areas of fusiform dilatation extending from the distal descending thoracic aorta superior to the renal arteries. Surgical therapy was undertaken to prevent rupture.
A left thoracoabdominal incision was performed and the chest was entered at the 6th intercostal space. The aorta was cross-clamped at the level of T5 and was transected. A 16mm woven Dacron tube graft was sutured end-to-end to the descending thoracic aorta, which measured 14mm, using “clamp-and-sew” technique. Intercostal arteries 8 and 9 were reattached by incorporation into the proximal anastomosis and intercostal artery 10 was ligated. The abdominal aorta was opened and a side hole was cut into the Dacron graft for reattachment of the celiac, superior mesenteric and bilateral renal arteries as a visceral patch. Histopathological examination of the resected aorta showed cystic medial necrosis with reactive adventitial vascular proliferation extending into the media and marked loss of elastic tissue and medial smooth muscle. His postoperative course was uneventful and he was discharged on postoperative day 5.
Imaging ten months later revealed aneurysmal dilatation involving the aortic segment proximal to the previous thoracoabdominal graft anastomosis. He underwent redo resection and graft replacement of the proximal descending thoracic aorta, which measured 7.2 cm at the level of T1 and 4.2 cm at the visceral patch (Fig. 2) via a left thoracoabdominal incision. Exploration revealed aneurysmal dilatation involving the aortic segment proximal to the previous thoracoabdominal graft anastomosis. Tuberous changes were noted at the proximal anastomosis leading to recurrent expansion and disruption. A 16mm woven Dacron tube graft was again used. Intercostal arteries 3 to 8 were ligated.
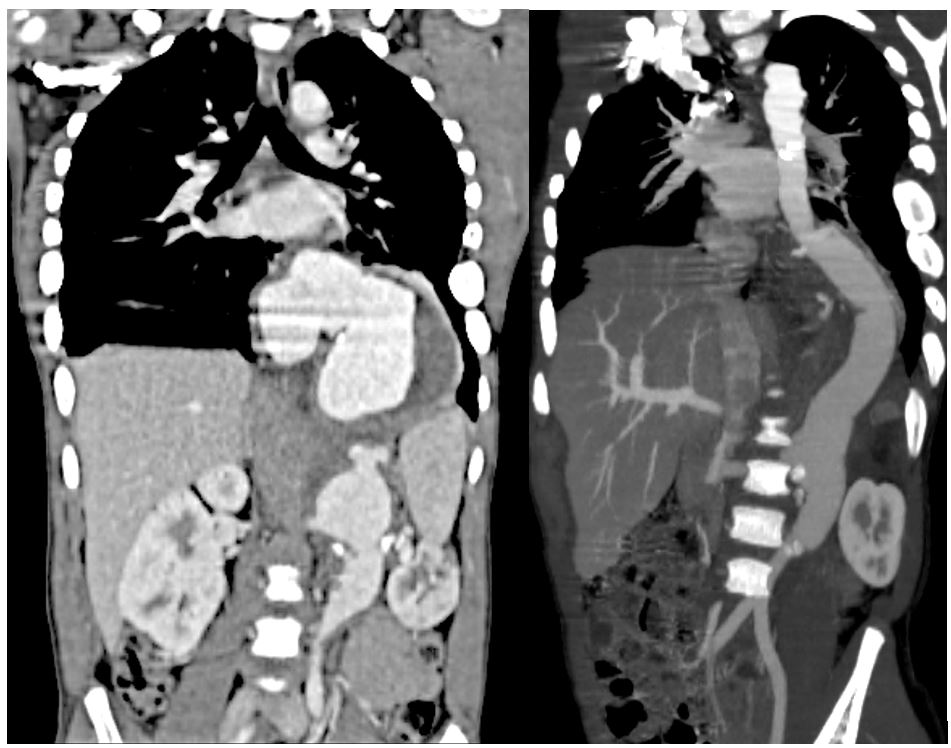
Figure 2 – Computed Tomographic Angiography ten months postoperative demonstrating 7.3 cm descending thoracic aneurysm and three months following descending aortic repair.
At nine years of age, surveillance imaging revealed an Extent IV TAAA with a 5.8 cm visceral patch aneurysm. He underwent redo resection and graft replacement using an 18mm woven Dacron tube graft via redo left thoracoabdominal exploration. Four side-branches with 8-mm woven Dacron were attached to the main body graft to prepare for the reconstruction for separate bypass to the celiac, superior mesenteric, right and left renal arteries (Fig. 3). Histopathological examination showed areas of normal aortic media with regions of excessive extracellular matrix deposition and nodules of smooth muscle cells (SMCs).
Discussion:
Abdominal aortic aneurysms in childhood are extremely rare and the majority of reported cases are associated with inherited disorders of connective tissues such as Marfan’s or Ehlers-Danlos syndromes (4). Tuberous sclerosis complex (TSC) is an autosomal-dominant genetic disease due to genetic mutations of the TSC1 and TSC2 genes, in which facial angiofibromas and hamartomas in multiple organ systems are common findings (5). Vascular aneurysms are an uncommon complication of TSC and can affect vessels of any size including the abdominal aorta and albeit more rarely, the thoracic aorta (6). Although significant vascular lesions are rare, when present they can be life threatening, thus recognition of TSC and early diagnosis of vascular involvement are important to prevent morbidity and mortality (7).
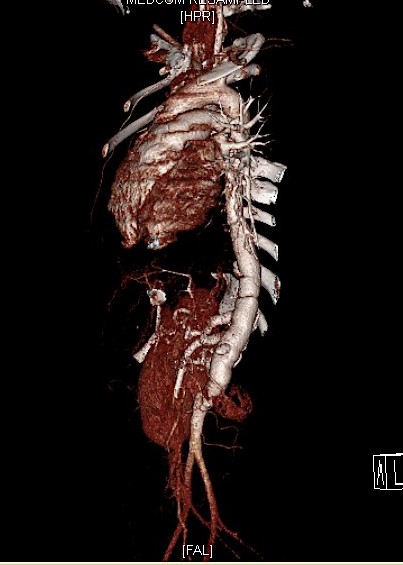
Figure 3 – 3-D reconstruction one month following visceral patch pseudoaneurysm.
The pathogenesis of aneurysm formation in TS is not fully understood, however dysplasia and medial atrophy contribute to the loss of aortic wall strength and aneurysm formation (8). Our patient’s pathology was significant for loss of elastic tissue and was notable for increased loss of SMCs in the media at the time of the third operation. The occurrence of a new aneurysm, superior or inferior to the graft after aneurysm repair, might be explained by an innate weakness of the aortic wall associated with TS (1).
In the present case, strict follow-up surveillance led to the incidental finding of an otherwise asymptomatic aneurysm, which prompted urgent re-exploration and repair. Due to the close proximity of the visceral and renal vessels, we performed island reconstruction as they were difficult to separate and anastomose individually to the aorta. It has been recommended to use the largest diameter graft that can be safely implanted, especially in infants and younger children, as larger conduits will allow for more growth before patients outgrow the initial graft, necessitating a second operation (7,8). We intentionally chose a 16mm graft for a 14mm mid-descending thoracic aorta during the first operation and an 18mm graft for a 16mm aorta during the third operation. Recent follow-up imaging demonstrated patent graft without aneurysmal changes.
References:
- S.-B. Moon, W.-Y. Shin, Y.-J. Park, S.-J. Kim. An Abdominal Aortic Aneurysm in an 8-Month-Old Girl with Tuberous Sclerosis. EJVES Extra, Volume 17, Issue 5, May 2009, Pages 45-47.
- Cao J, Gong L, Guo DC, et al. Thoracic aortic disease in tuberous sclerosis complex: molecular pathogenesis and potential therapies in Tsc2+/- mice. Hum Mol Genet.
- Calcagni, G., Gesualdo, F., Tamisier, D., Brunelle, F., Sidi, D., & Ou, P. (2008). Arterial aneurysms and tuberous sclerosis: A classic but little known association. Pediatric Radiology, 38(7), 795–797.
- Rutherford RB: Vascular Surgery. Philadelphia, PA, Saunders, 1985, pp 750-751.
- Eliason, Jonathan L. et al. Surgical Treatment of Abdominal Aortic Aneurysms in Infancy and Early Childhood. Journal of Vascular Surgery, Volume 64, Issue 5, 1252 – 1261
- Rolfes DB, Towbin R, Bove KE. Vascular dysplasia in a child with tuberous sclerosis. Pediatr Pathol 1985;3:359-373.
- Boronat, S, Barber, I. Less common manifestations in TSC. Am J Med Genet Part C. 2018; 178C: 348– 354.
- Jost CJ, Gloviczki P, Edwards WD, Stanson AW, Joyce JW, Pairolero PC. Aortic aneurysms in children and young adults with tuberous sclerosis: a report of two cases and review of the literature. J Vasc Surg 2001;33:639-64.