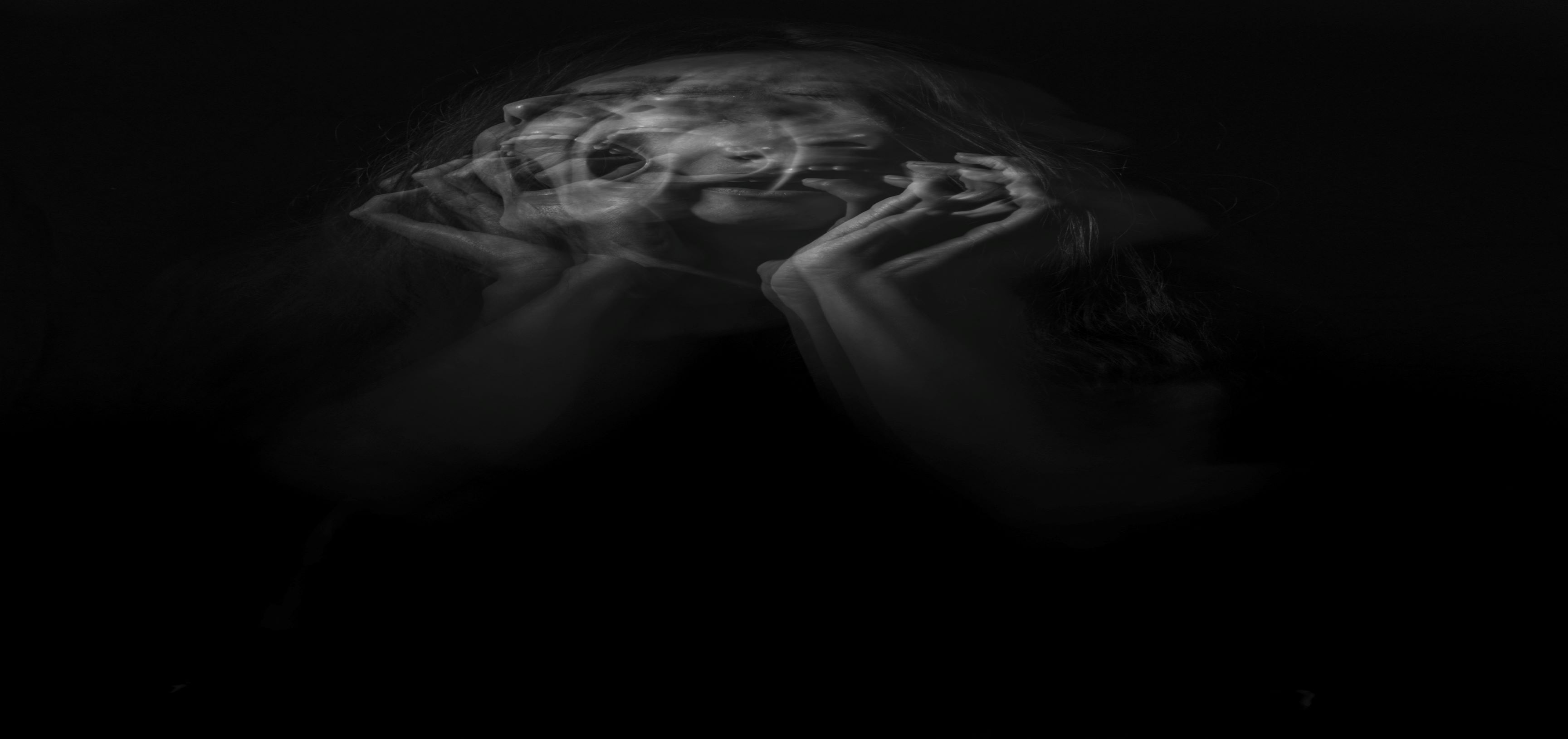
Suicide in bipolar disorder
Written by: Gabriel Fries, PhD, MSc
Being among the top 10 leading causes of death in the United States and the world, suicide is considered a major public health issue and a complex multifactorial human behavior. Studies suggest that the great majority of suicide cases occur among subjects with major mental illness, mainly mood disorders, with the risk of suicide death being 10-30 times higher in patients with bipolar disorder than in the general population. Specifically, it is estimated that 20-60% of patients with bipolar disorder attempt suicide at least once in their lifetime.
The high prevalence of suicide and suicide attempts and the burden it causes to patients and family members make it imperative for us to investigate it, identifying its risk factors to allow for early identification and prevention. In patients with bipolar disorder, factors that have been shown to increase suicide risk include a history of previous suicide attempt, family history of suicide and mood disorder, frequent prior hospitalizations, early age at onset of the illness, rapid-cycling course, predominant depressive polarity, long duration of untreated illness, occupational problems and unemployment, adversities in personal history (childhood trauma, for example), impulsive and aggressive traits, among others. In addition, the time period immediately after discharge from a psychiatric hospitalization, the period immediately after hospital admission, and the early years after receiving the diagnosis have been characterized by extremely high levels of suicide activity.
All in all, clinicians are trained to assess suicide risk by identifying many of these risk factors and performing comprehensive examinations of the mental state in patients. However, not all patients with bipolar disorder that present identifiable risk factors will engage in suicidal behaviors, and many patients who express suicidal ideation may attempt to commit suicide. At the same time, many patients who eventually commit suicide may do it without communicating any suicidal ideation (Malhi et al., 2018). This suggests the need for the identification of biological markers that can be used concomitantly to clinical assessments for an improved suicide risk prediction and management in patients.
Funded by the National Institute of Mental Health (NIMH), the Translational Psychiatry Program in our Department is starting a research project aimed at identifying so-called “epigenetic markers” in post-mortem brains of patients with bipolar disorder who committed suicide or died of other causes. ‘Epigenetics’ refers to processes that can change the activity of our DNA (normally in response to environmental stimuli) without changing its sequence. Accordingly, many previous studies have suggested that epigenetics may be a key molecular underpinning of the suicide activity, although such a direct investigation in a large number of brains from suicide patients with bipolar disorder has never been performed. With this translational study, we aim to integrate expertise in both clinical and basic sciences to generate useful hints at the biology of suicide in bipolar disorder and ultimately contribute to its effective prediction and prevention in this vulnerable population.
References:
Malhi GS, Outhred T, Das P, Morris G, Hamilton A, Mannie Z. Modeling suicide in bipolar disorders. Bipolar Disorders, 20(4):334-348, 2018.
Dome P, Rihmer Z, Gonda X. Suicide risk in bipolar disorder: a brief review. Medicina, 55:403,