Stewart Cardiovascular Imaging and Therapeutic Innovation Laboratory
About our lab
The Stewart Cardiovascular Imaging and Therapeutic Innovation Laboratory is staffed by specially trained investigators including physicians and veterinary staff to provide high quality care and convenience for research studies of heart and vascular diseases. Equipped with the latest technological advancements, not only do you have the most innovative fluoroscopic imaging at your fingertips, you will also have the ability to image three dimensionally without ever moving the subject.
Our focus areas
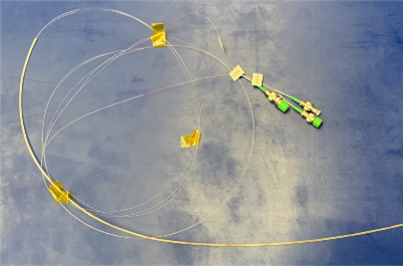 Fiber Optic Shape Sensing for Interventional Guidance. The shape sensor (i.e. Multiplanar Position and Force Sensing Catheter) employs multiple sets of fiber optic sensors that modulate wavelengths of light to detect deformations in endovascular tools. This sensor data enables real-time visualization and computation of the wire’s 3D shape, which complements existing imaging techniques like ultrasonic and fluoroscopic imaging. By registering the computed shape with the patient’s anatomical 3D model, interventionalists can more accurately determine the proximity of endovascular tools to cardiac structures during procedures. We are currently working on ways to include force sensing and so far have outperformed other approaches described in the state-of-the-art literature. This development will lead to more advanced applications to actual delivery systems used in structural heart interventional procedures.
Fiber Optic Shape Sensing for Interventional Guidance. The shape sensor (i.e. Multiplanar Position and Force Sensing Catheter) employs multiple sets of fiber optic sensors that modulate wavelengths of light to detect deformations in endovascular tools. This sensor data enables real-time visualization and computation of the wire’s 3D shape, which complements existing imaging techniques like ultrasonic and fluoroscopic imaging. By registering the computed shape with the patient’s anatomical 3D model, interventionalists can more accurately determine the proximity of endovascular tools to cardiac structures during procedures. We are currently working on ways to include force sensing and so far have outperformed other approaches described in the state-of-the-art literature. This development will lead to more advanced applications to actual delivery systems used in structural heart interventional procedures.-
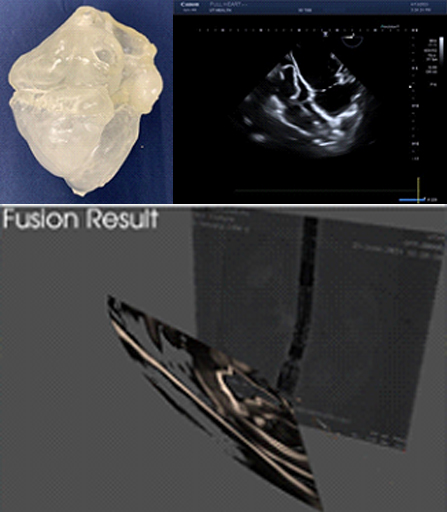
(Left) Phantom heart made from ballistic gel. (Right) 2D TEE scan of the heart in 4 chamber view. (Bottom) Work in progress of fusing 2D TEE scan with fluoroscopic image.
Multimodality Fusion Imaging. Despite the great benefits provided by transcatheter procedures, an ongoing challenge is the need for visualization of delivery devices during the procedure. Intraoperative imaging is currently performed with fluoroscopy and echocardiography. Each modality provides a unique perspective into the anatomy and relative positioning of delivery devices. A difficult-to-develop skillset is the mental integration of vastly different types of imaging information towards accurately guiding delivery systems during an interventional procedure. The time taken to understand the different imaging data increases radiation exposure, which is harmful to both the physician team and the patient. One approach to improve visualization is to fuse imaging information into a single image. We are now working towards building in-house capabilities to fuse the following information: fluoroscopic imaging, echo imaging, pre-operative 3D CT models, and 3D shape sensing from the Smart Wire. So far, we have demonstrated the fusion of echo and 3D CT and are now working on echo-fluoro fusion. We are building our own phantom heart models from patient CT data to perform experiments. In this project, the spin-scan ability of the C-arm in the Stewart lab will replace traditional CT imaging.
-
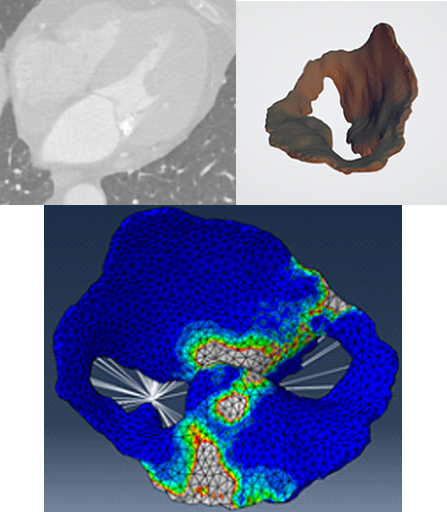
Figure 3. (Left) CT scan from de-identified patient. (Right) 3D model derived from CT volume. (Bottom) Finite element analysis of leaflet stresses after applying boundary conditions and pressures.
Finite element modeling of mitral valve to optimize Mitra clip delivery. We are working on the finite element modeling of the mitral valve apparatus and the effects of different interventional devices on the stresses of the mitral valve leaflets. Knowing the stresses may help elucidate the short- and long-term response of mitral valve physiology to different therapies. The work involves the application of the correct constitutive equations for material behavior and the implementation of the correct boundary conditions to simulate the true situation. The highly active cath lab allows access to a large library of patient anatomies and expertise in transcatheter procedures. The results from this contribution will help improve patient outcomes and effectiveness of related interventional procedures.
Animal studies
Animal work is performed in the Animal Care Center (ACC) of McGovern Medical School at UTHealth Houston. Fully accredited with AAALAC, the CLAMC animal resources provides professional veterinary, surgical and animal care services, and its staff includes five veterinarians, seven veterinary technicians, and over thirty animal care and support personnel. The rooms are modern climate controlled with facilities for diagnostic procedures, isolation treatment, and necropsies are available.
Main angiographic experimental and surgical lab
600 square feet of experimental space in an accredited facility.
5-axis flat panel digital radiographic system with 3D acquisition reconstruction and analysis:
- 3D acquisition
- CT-like imaging
- Rotational DA/DSA
- Stepping DSA
- 2D/3D road map
- Online aortic valve analysis
- Software for TAVR
- Fusion fluoroscopic live imaging
- IVUS system analysis
- Anesthesia machine with full availability of medical gasses
- Advanced surgical instruments
- Access to 2D/3D TTA Echo Machines
Tissue analysis lab
- Apoptosis Analysis
- RIA Peptide Assays
- Radioactive Microsphere Blood Flow Analysis
- Heart tissue Isolation Techniques
- Protein Assays
- Infarct Size Analysis
- Pathology Core Laboratory Histology
- Calcium Influx Analysis
History of the lab
- Established in 1980 with conversion to an all-digital lab in 1994.
- Participated in the pioneering and pre-clinical development of Percutaneous and implantable Left-Ventricular Assist Devices.
- Pioneered the development and testing of new interventional cardiac devices including guide wires, guide catheters, balloons, stents, atherectomy systems and intravascular imaging systems.
- In addition to cardiac device development and testing the lab has also focused on coronary physiological studies, particularly in the area concerning salvage of ischemic myocardium.
- Over 300 scientific publications have been generated by the research conducted in our laboratory.
About Dr. Richard Smalling
 Dr. Smalling is a native Texan who received his undergraduate degree in Aerospace Engineering, master’s degree in Bio-Medical Engineering, and Ph.D. from The University of Texas. He is an AOA graduate of The University of Texas Medical School at Houston and completed residency training and cardiology fellowship at University of California San Diego. Dr. Smalling is board certified in internal medicine, cardiovascular medicine, and interventional cardiology
Dr. Smalling is a native Texan who received his undergraduate degree in Aerospace Engineering, master’s degree in Bio-Medical Engineering, and Ph.D. from The University of Texas. He is an AOA graduate of The University of Texas Medical School at Houston and completed residency training and cardiology fellowship at University of California San Diego. Dr. Smalling is board certified in internal medicine, cardiovascular medicine, and interventional cardiology
Dr. Smalling specializes in coronary artery angiography and revascularization, treatment of adult congenital heart disease percutaneously, and the treatment of vascular heart disease percutaneously. He has extensive expertise in the treatment of peripheral vascular disease including carotid stenting, percutaneous endovascular repair of abdominal aortic aneurysm, renal, iliac, femoral and below-knee angioplasty and stenting. Additionally, his team is experienced in utilizing left ventricular assist devices to support high risk coronary angioplasty and complicated valve treatment procedures.
Contact Us
Learn more about the Stewart Cardiovascular Imaging and Therapeutic Innovation Laboratory today. Contact us for partnership and collaboration opportunities.
