Adolescent Idiopathic Scoliosis
Overview
Adolescent Idiopathic Scoliosis (AIS) is a common spinal deformity that typically emerges during adolescence, most commonly between the ages of 10 and 18. It is characterized by an abnormal lateral curvature of the spine, often accompanied by vertebral rotation. “Idiopathic” means that the exact cause of AIS is unknown, though several factors are believed to contribute to its development.
More information on Adolescent Idiopathic Scoliosis:
-
Prevalence: AIS is the most common type of scoliosis, accounting for about 80% of all scoliosis cases. It affects both boys and girls, but girls are more likely to progress to a severe curve.
- Cause: While the exact cause of AIS remains unclear, it is believed to be influenced by a combination of genetic, environmental, and hormonal factors. There seems to be a genetic predisposition, as AIS often runs in families.
- Symptoms: The most common symptom of AIS is an abnormal curvature of the spine, which can result in an uneven shoulder and hip alignment. Other symptoms may include back pain, muscle imbalances, and, in more severe cases, respiratory or cardiac problems if the curvature puts pressure on the lungs or heart.
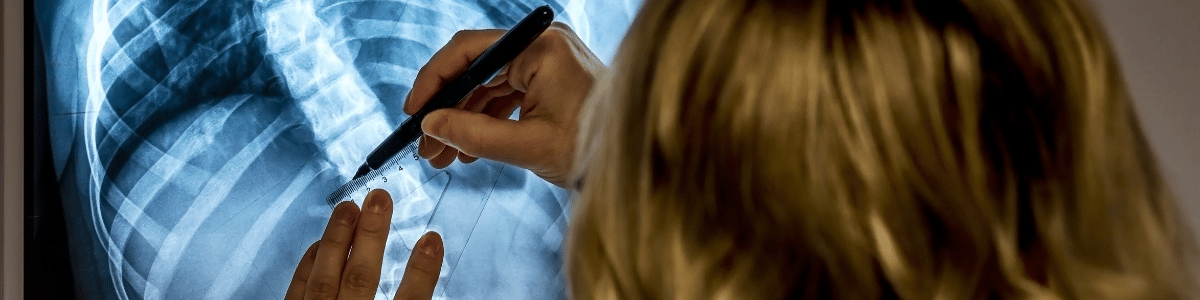
- Diagnosis: AIS is typically diagnosed through a physical examination and an X-ray to assess the degree and location of the spinal curvature. Early detection is essential to monitor the progression and start appropriate treatment.
- Treatment: Treatment options for AIS depend on the severity of the curvature, the patient’s age, and other factors. Treatment options may include observation, bracing, or in some severe cases, surgery. The goal of treatment is to prevent the progression of the curve and manage any associated symptoms.
- Prognosis: The prognosis for AIS varies depending on the severity of the condition and the age of the patient. Mild cases may not progress significantly and may not require treatment. However, more severe cases can worsen over time and may need surgical intervention to correct the curvature.
- Psychosocial Impact: Adolescents with AIS may experience psychosocial challenges due to their appearance and potential limitations caused by the condition. Support and education are often provided to help these individuals cope with the emotional and social aspects of AIS.
Early detection and timely intervention play a crucial role in managing AIS effectively. Regular monitoring and treatment can help prevent the condition from worsening and reduce the impact it has on a person’s quality of life.
Imaging
Treatment
Surgical treatment for Adolescent Idiopathic Scoliosis (AIS) is typically considered when the spinal curvature is severe, progressing rapidly, or when other non-surgical treatments like bracing have not been effective. The primary goals of surgery for AIS are to correct the curvature, stabilize the spine, and prevent further progression. There are several surgical options for treating AIS, and the choice of procedure depends on various factors, including the severity of the curvature, the age of the patient, and individual considerations. Here are some common surgical options:
- Spinal Fusion Surgery: Spinal fusion is the most common surgical procedure for AIS. It involves fusing together two or more vertebrae to straighten the spine and prevent further curvature progression. During the procedure, the surgeon typically uses bone grafts or bone substitutes to promote fusion, and they may also use metal rods, hooks, wires, or screws to hold the spine in the corrected position. Spinal fusion provides a permanent correction of the curvature but limits the mobility of the fused spinal segments.
- Thoracoscopic Anterior Spinal Fusion: This minimally invasive approach involves accessing the spine through small incisions in the chest, often on the patient’s side. It allows for correction of the curvature from the front (anterior) of the spine and can result in less visible scarring and a potentially shorter recovery period compared to traditional open surgery.
- Hemivertebrae Resection: In cases where AIS is caused by congenital hemivertebrae (abnormal half-shaped vertebrae), surgical resection of the affected vertebrae may be necessary. This procedure can involve removing the deformed vertebra and fusing the surrounding vertebrae to correct the curvature.
- Growing Rods: Growing rods are often used in younger patients with AIS who are still growing. These are adjustable rods attached to the spine that allow for gradual correction of the curvature as the child grows. Periodic lengthening of the rods is needed to accommodate growth.
- Vertebral Body Tethering: Vertebral body tethering is a newer, less invasive surgical technique. It involves attaching a flexible cord or tether to the vertebral bodies to partially correct the curvature while allowing for continued spinal growth. This procedure may be an option for some AIS patients, especially those who want to maintain more mobility in their spines.
- Posterior Spinal Fusion with Instrumentation: This is the traditional approach to spinal fusion for AIS. It involves accessing the spine through an incision in the back (posterior) and fusing the affected vertebrae using metal instrumentation. Modern techniques use advanced materials and technology to reduce the impact of surgery and promote a faster recovery.
The choice of surgical approach and specific procedure depends on individual patient factors, including the severity and location of the curvature, the patient’s age, and their overall health. It’s important for patients and their families to discuss the available options, potential risks, and expected outcomes with our surgeons. Surgical treatment for AIS is generally considered a last resort when non-surgical methods are ineffective, and it’s crucial to carefully weigh the risks and benefits before making a decision.