George Williams, MD
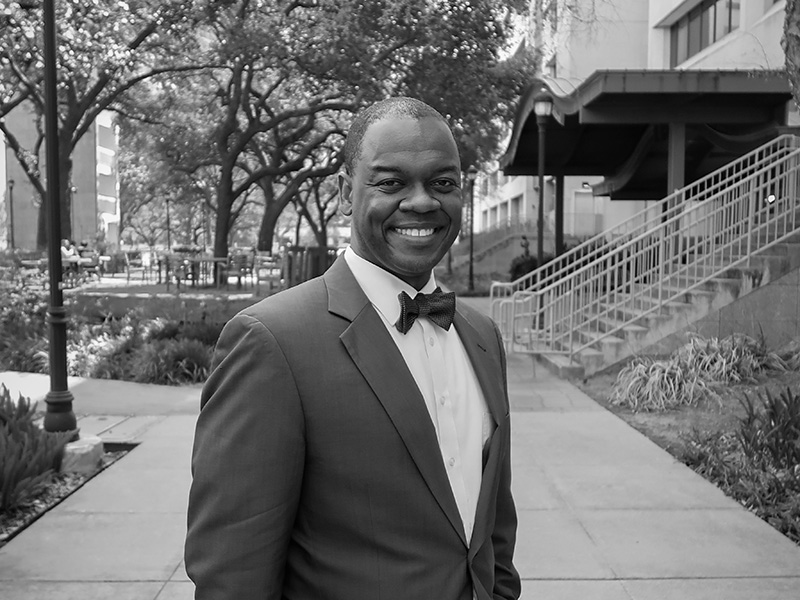
Associate Professor
Department of Anesthesiology and Critical Care Medicine
It started at the end of March/beginning of April, once it became clear that COVID was coming to the United States, and we had to be prepared. It seemed like our life stopped and everything went to planning and meetings, planning and meetings. We had about 5 hours of meetings in a day on top of normal clinical obligations, which made it difficult. Everything you were doing had to take a backseat – even if it was a bill or something for your house, anything. I remember going from some stage like ‘let it come, we are ready.’ Then we started having some patients, and it started building.
My patient population is multi-surgical patients, and as anesthesiologists, we are the ones intubating. There was a lot of concern about undiagnosed COVID patients in the community, and intubation is the highest risk procedure in terms of getting exposed to COVID. The operating rooms were still going, and we couldn’t test everyone. On the ICU side we took one, two patients and seemingly overnight we have all of these COVID patients. So, in the span of 3 months, we went from extreme planning to extreme clinical volume that was affecting everything.
One of the most interesting clinical effects was that we became afraid to have our trainees help out with patient care. So, you have a resident whose job it is to take care of patients in the operating room, and they can’t intubate anymore, they can’t extubate anymore, everyone has to leave the room and only the attending can provide the care. In the ICU, we are afraid to let them see the patients, no medical students can come in. We transitioned from this robust academic practice teaching everything we do to apologizing multiple times a day for not letting our trainees do anything.
“I’m very grateful and glad I was here for this.
I know it was something I was supposed to do, and I’m really grateful I get to do what I love.”
Then we got deep into the PPE conundrum. That happened when patients came in, and we couldn’t order anymore. A lot of people in the community got creative. One of the things that was very special to me was when a fraternity created and delivered an acrylic intubating box to us at LBJ Hospital. They had seen online how helpful it would be. I got my first cloth face mask from a Vietnamese church; people brought lunch to the whole hospital. It was so special because it was a very scary time.
I didn’t realize how stressful it was going through it, because I compartmentalize things and have always felt like a strong person. But, it can really affect you. It became an extreme situation for me when we had a case with a young mom who had COVID who did not survive but whose baby did following a C-section. Once that happened, then it really jelled to me as a person – this is not normal stuff. Then there became a series of experiences like that, there’s someone who looks like someone you know who has a young family, someone wants to visit their family but they can’t. You consult other doctors, and they are afraid to see patients. You see people leaving the hospital carrying boxes of toilet paper. All of these ethical constructs and contracts – these norms breaking down around you at the same time we are providing care, and we have to stay focused on that.
Once we got past six months, after we got past the surge, things almost became normal. We got used to lots of COVID patients, we created extra ICUs, and got called to help in other places. We were called to help in other Hermann Hospitals – other ICU doctors had gotten sick. People we had no existing relationships with, we had never met before, but every time they called us to help, we went. Those barriers in the community that we had had – me versus you – in that situation, there was no time for that. Everyone was trying their very best, whatever we can do, all hands on deck. Some residents went to our ICUs to help out. We put together some emotional support to help them cope with the number of fatalities – something that used to be just on paper has become a really functional system because we had to.
From the 6- to 12-month period, the biggest pattern I saw was trying to engage the public more. We are trying to educate about social distancing and now vaccine hesitancy. We are also making sure we can get back to our academic mission and what’s important, because before you know it, another 6-12 months have gone by. We’ve barely been able to work on our papers, on excellent teaching, it’s all just about keeping up. It was a tangible experience to see what our practice would be like if education wasn’t front and center. That is not our culture.
It’s been an interesting year for all of those reasons. There have been challenges personally, psychologically, clinically, but also challenges meeting our mission, being a benefit to the public, dealing with the constructs we all take for granted in our community and with our society being intact. I’m very grateful and glad I was here for this. I know it was something I was supposed to do, and I’m really grateful I get to do what I love. Getting a chance to do what you love is so special and rare, and I got a chance to put everything out there to help as much as I could.
