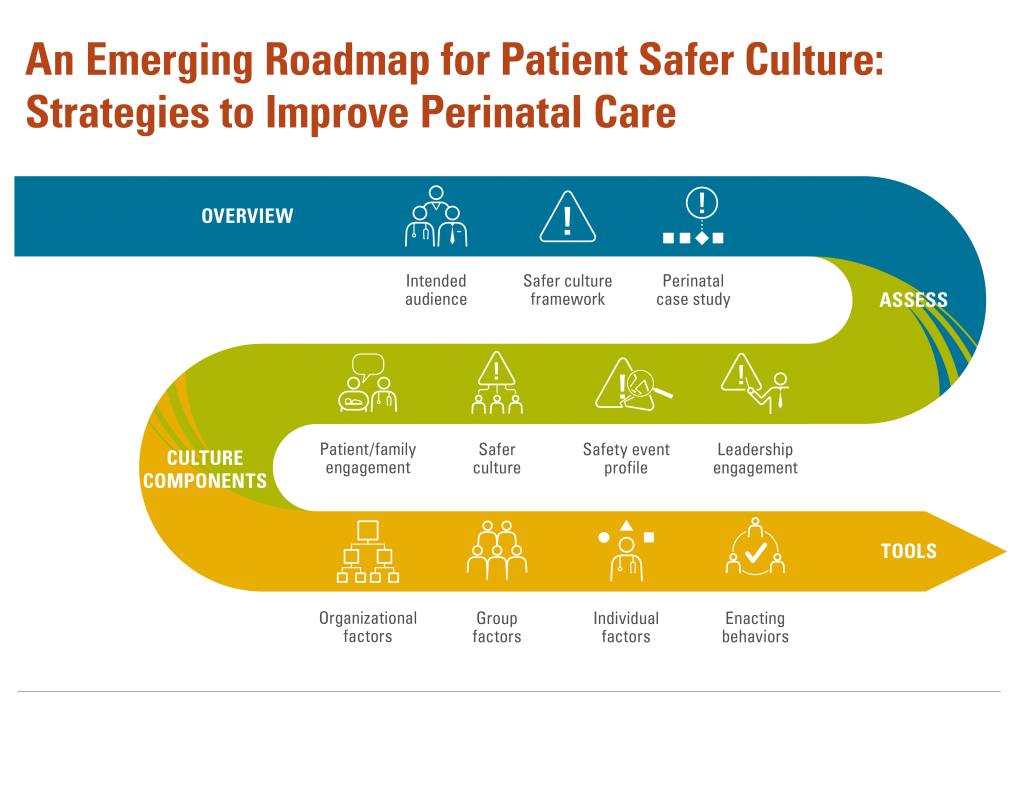
Safer Culture Roadmap
A roadmap for your journey to creating an effective patient Safer Culture
Organizations can use this roadmap to guide individuals’ groups’, and leaders’ efforts to improve Safer Culture by understanding assessing, measuring, and improving all of the components required for an effective patient Safer Culture.