Safer Culture Framework
Safer Culture » INSIDE THE PROJECT » Safer Culture Framework
The Safer Culture Framework
Defining the conditions that create and sustain Safer Culture
Our goal in promoting a perinatal Safer Culture is preventing serious maternal events. To define the necessary components of an effective Safer Culture, we reviewed literature and examined frameworks from many industries where safety is a priority — aviation, aerospace, nuclear energy, and other high-reliability organizations. We sought to identify existing tools (measures, interventions and resources) that organizations can use to measure and improve Safer Culture.
The Functional Framework for Safer Culture details the foundational enabling factors that create the ideal conditions for an organization’s individual employees, groups, and leadership to adopt Safer Culture. The underlying assumptions, values, and norms of Safer Culture are manifested in employee behaviors, which in turn influence safety outcomes. Employees then learn from these safety outcomes to feed back into reinforcing the Safer Culture.
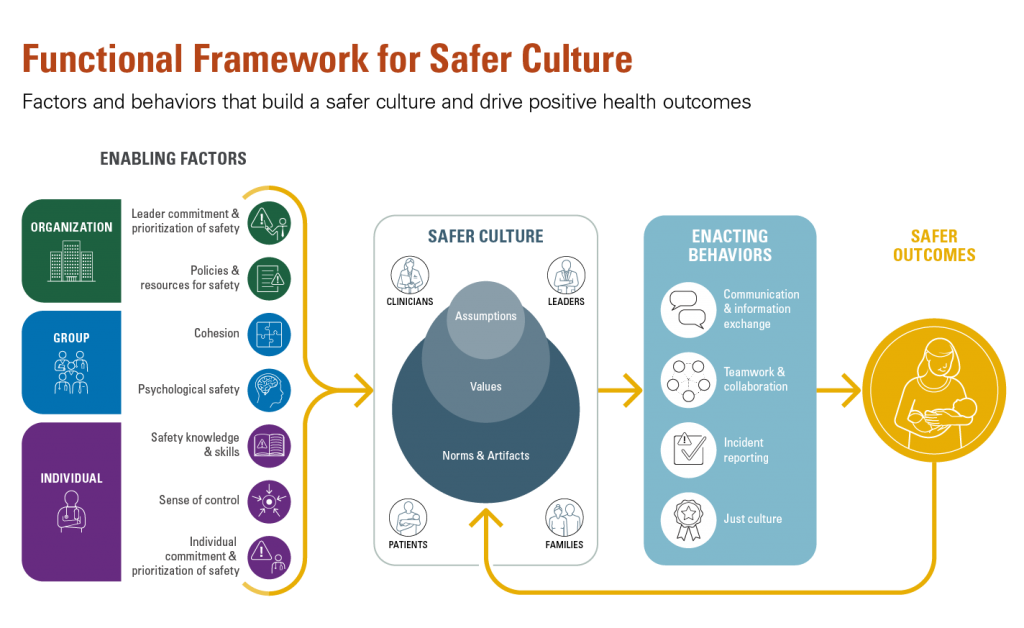
Factors and Behaviors that build a safer culture and drive positive health outcomes
Note: Figure adapted from Bisbey et al. (2019)
Enabling factors
The Safer Culture framework identifies seven enabling factors that form the foundation of Safer Culture. These seven enabling factors are grouped within three categories:
- Organization (leadership commitment and policies/resources dedicated to safety)
- Group (cohesion and psychological safety)
- Individual (knowledge of safety, sense of control and commitment to safety)
Each enabling factor, or building blocks of Safer Culture, represents an essential component influencing the culture. Enabling factors set the context for the norms, values, and assumptions about safety that must take hold within the organization.
Evidence shows that a positive patient Safer Culture can only arise when each factor is present concurrently:
| DEFINITIONS AND HEALTHCARE-RELEVANT EXAMPLES | ||
| FACTOR | DEFINITION | HEALTHCARE APPLICATION/TOOLS FOR TOOLKIT |
| ENABLING FACTORS | factors that provide the necessary context for norms, values, and assumptions around safety to develop |
|
| ORGANIZATION | factors that impact all members within an organization or department to a similar degree |
e.g., hospital, emergency department, cardiac unit, ICU |
| Leader commitment & prioritization of safety | leadership is perceived to hold a priority of safety over all other performance goals (e.g., profit, speed) |
Governing boards, executive leaders, and unit leaders all verbalize and demonstrate a commitment to safety.
Potential Tools:
|
| Policies and resources for safety | policies and resources provided by the organization concerning safety (e.g., training resources, maintained equipment, safety policies and protocols |
The organization has policies intended to support the delivery of safe patient care such as policies about just culture, safety event reporting, behavior expectations, and evidence-based safety practices. Resources would include support for data analysts who can access data in the EHR to monitor and improve safety, expertise in safety science, process improvement, leadership development, etc.
Potential Tools:
|
| GROUP | factors that impact all individuals within a team or group to a similar degree, and may differ across teams/ groups |
e.g., OR team , primary care team |
| Cohesion | commitment to the group and its goals, as well as pride for the groups values and perceived importance of being a member |
Each member of the group (OR team) commits and willingly complies with patient safety initiatives such as doing the time out for surgical checklist.
Potential Tools:
|
| Psychological safety |
a collective perception that the group is safe for interpersonal risk taking and can speak up without fear of embarrassment, punishment, or ridicule |
Staff willingly report variances in care and participate in multidisciplinary debriefings about safety events that occur on their unit.
Potential Tools:
|
| INDIVIDUAL | factors that may differ from person to person within the organization |
e.g., fellows, residents, interns, staff, contractors, patients and families |
| Safety knowledge & skills |
the ability to recognize safety threats, understand their origins and carry out procedures to address them effectively |
Clinicians, patients and families have the knowledge to report safety threats and participate in quality initiatives to correct these threats.
Potential Tools:
|
| Sense of control | the belief that ones behavior has the potential to impact important outcomes |
Clinicians, patients and families comply with completing surveys assessing their attitudes about safety outcomes.
Potential Tools:
|
| Individual commitment & prioritization of safety | a positive attitude and motivation towards safe operations, and a priority of safety over all other performance goals |
Clinicians participate in daily huddles about patient safety issues and discuss patient safety on rounds.
Potential Tools:
|
Enacting Behaviors
The Safer Culture created by an organization’s leaders, groups, and individuals determine the type of enacting behaviors the organization adopts to promote and ensure safe care. Enacting behaviors are the behavioral expressions of held assumptions, values, and norms about safety.
The four most common enacting behaviors for safety are:
- Communication and information sharing
- Incident reporting
- Teamwork and collaboration
- Fairly rewarding and punishing its members for safety outcomes
| DEFINITIONS AND HEALTHCARE-RELEVANT EXAMPLES | ||
| FACTOR | DEFINITION | HEALTHCARE APPLICATION/TOOLS FOR TOOLKIT |
| ENACTING BEHAVIORS | behavioral expressions of held assumptions, values, and norms around safety |
|
| Communication & information exchange | the exchange of information between individuals and/or teams, and the extent to which messages are effectively sent and received |
Handoffs among clinicians regarding patient status, transitions of care (inpatient to rehabilitation, intensive care to general ward, inpatient to outpatient primary care.Potential Tools:
|
| Teamwork & collaboration | observable behaviors groups enact in efforts to collaborate towards task goals (e.g., monitoring, providing backup, goal-setting and planning, coordinating) |
Operative room teams, ward teams, labor and delivery teams that exhibit appropriate teamwork behaviors.
Potential Tools:
|
| Incident reporting | engaging in reporting when an error or near-miss occurs that has safety-related consequences |
Clinicians use the organization’s incident reporting system to report patient safety events.
Potential Tools:
|
| Fair rewarding and punishing | rewarding desired/effective behaviors and enforcing fair, non-punitive consequences for errors. Should not be excessively punitive nor lenient |
Clinicians who commit typical errors are not punished but instead contribute to learning from the errors. Clinicians who intentionally violate policies known to improve safety, or who exhibit other unprofessional behavior are punished.Potential Tools:
|