Controlled Resuscitation in Trauma Patients Clinical Practice Guideline
Original Date: 06/2017 | Last Review Date: 09/2020
Purpose: To standardize blood pressure goals in bleeding trauma patients undergoing active resuscitation.
Recommendations
| Patient population | Recommendation |
|---|---|
| Adult blunt trauma patient without known traumatic brain injury | Resuscitate to a SBP >70 mmHg until hemorrhage is controlled |
| Adult penetrating trauma patient without known traumatic brain injury | Resuscitate to a MAP > 50 mmHg or SBP >70 mmHg until hemorrhage controlled |
| (GRADE Level of Quality – moderate; USPSTF strength of recommendation – B [intervention is recommended]) | |
*Note: there is increasing interest in and use of resuscitative balloon occlusion of the aorta (REBOA). When used correctly, REBOA dramatically decreases blood pressure distal to the site of hemorrhage and, as such, is complimentary to controlled resuscitation, not contradictory.
Summary of Recommendations/Guideline
For hypotensive patients arriving to the trauma center with penetrating or blunt trauma, resuscitation should be titrated to a systolic blood pressure >70 mmHg until ongoing hemorrhage has been ruled out or control of hemorrhage has been obtained. These patients should receive early blood product utilization and minimal crystalloid. Once rTEG data is available it should be used to further guide resuscitation strategies.
Summary of Public Health Impact
In 2013, injury was the most common cause of death among people ages 1-44 years, accounting for 59% of all deaths in this age range. There were over 192,900 deaths from injury, approximately one every 3 minutes1. Since trauma is a disease of the young, injury accounts for the most life-years lost than any other disease – 30% of all life years lost in the U.S. compared to cancer 16% and heart disease 12%.2
Truncal hemorrhage accounts for 20-40% of trauma deaths occurring after hospital admission and continues to be a leading cause of potentially survivable deaths. 3,4 This is despite a significant amount of time and healthcare resources attempting to address this problem, including: implementation of trauma systems 5, utilization of in-house trauma surgeons , and development of hemostatic resuscitation,7 to name a few.
Non-compressible torso hemorrhage (NCTH) occurs from intrathoracic, intraabdominal, and/or pelvic injuries. Identification of NCTH can be difficult. Additionally, obtaining control of hemorrhage once diagnosed requires invasive procedures and time to expose the source of bleeding. NCTH is reported to have a mortality rate of 45% in civilian Level 1 trauma centers.8
Until the recent wars in Iraq (2003-2010) and Afghanistan (2001-2014), the prompt administration of isotonic crystalloid was considered standard of care for hypotensive trauma patients, including those with NCTH.9 Indeed, the Advanced Trauma Life Support (ATLS) course recommended two liters of crystalloid until the most recent edition (9th edition), in which the amount of crystalloid was reduced to one liter.
This practice has come into question, however, after multiple animal models have shown increased hemorrhage when the animal is resuscitated with higher volumes of crystalloid and to higher levels of systolic blood pressure.10,11 These findings led to the clinical interest of controlled resuscitation (also known as hypotensive resuscitation, delayed resuscitation, or permissive resuscitation) – the idea of delaying resuscitation or resuscitating to a lower than normal mean arterial pressure or systolic blood pressure until hemorrhage is ruled out or surgically controlled.
A key differentiation in studying this subject is the stratification by mechanism of injury. A patient with blunt injury (e.g. motor vehicle crash, motorcycle crash, fall) requiring laparotomy for truncal injury is more likely to have concomitant extra-truncal injuries, including traumatic brain injury, than a patient with a penetrating truncal injury (e.g. gunshot wound, stab wound). A key tenet of care in a patient with traumatic brain injury is avoidance of hypotension, thus permissive hypotension may be harmful in this subset of patients.
Primary Question:
Among hypotensive, adult trauma patients, does controlled resuscitation (permissive hypotension) until hemorrhage is stopped decrease in-hospital mortality?
Population – adult trauma patients without evidence of traumatic brain injury
Intervention – controlled resuscitation (permissive hypotension) until hemorrhage is controlled
Control – standard of care resuscitation
Outcome – in-hospital mortality
Because of the significance of the mechanism of injury on the possibility of traumatic brain injury, the primary question must be categorized by mechanism and injury pattern:
Key Questions to Consider:
- In patients with penetrating trauma, does controlled resuscitation (permissive hypotension) until hemorrhage is stopped decrease in-hospital mortality?
- In patients with blunt trauma, does controlled resuscitation (permissive hypotension) until hemorrhage is stopped decrease in-hospital mortality?
Methods
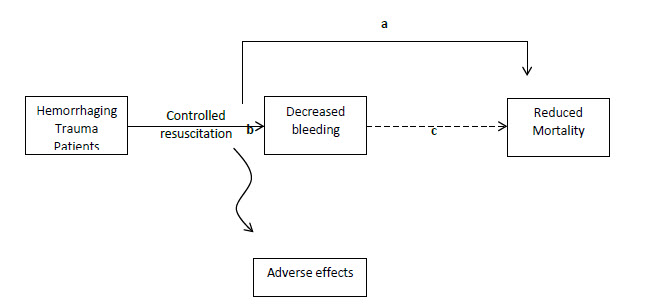
To answer these questions, our systematic review must identify evidence that controlled resuscitation (permissive hypotension) either (a) directly reduces mortality or (b) directly reduces the amount of hemorrhage.12 It is reasonable to assume an association between decreased bleeding (theoretical intermediate outcome) and reduced mortality.
Search Strategy
Inclusion criteria:
- Adult trauma patients
- Blunt or penetrating mechanisms of injury
- Outcome = in-hospital mortality
- Randomized controlled trials
- English language
- Human subjects
Databases and Search Terms:
- Pubmed:
- (“delayed resuscitation” OR “hypotensive resuscitation” OR “controlled resuscitation”)
- (“delayed resuscitation” OR “hypotensive resuscitation” OR “controlled resuscitation”) AND (Hospital Mortality OR Hypotension/mortality OR Treatment Outcome OR Survival Rate) AND (Abdominal Injuries/surgery OR Wounds, Nonpenetrating/therapy OR Wounds, penetrating/surgery OR Multiple trauma/surgery OR Multiple trauma/mortality)
- Scopus:
- (“delayed resuscitation” OR “hypotensive resuscitation” OR “controlled resuscitation”) AND trauma
- Cochrane Database:
- (hypotensive resuscitation OR delayed resuscitation OR controlled resuscitation) AND trauma
- Embase:
- hypotensive AND resuscitation OR delayed AND resuscitation OR controlled AND resuscitation AND trauma AND [humans]/lim AND [English]/lim AND (‘randomized controlled trial (topic)’/de OR ‘systematic review’/de)
- Published abstracts of the following national trauma associations:
- The American Association for the Surgery of Trauma (https://www.aast.org/annual-meeting/past-and-future-meetings/search-meeting-abstracts)
- The Eastern Association for the Surgery of Trauma (https://www.east.org/education-career-development/annual-scientific-assembly/annual-scientific-assembly-archive)
- The Western Trauma Association (https://www.westerntrauma.org/previous-annual-meetings/)
- Podium presentation, quick shots, and posters searched for following terms: hypotensive OR hypotension OR resuscitation
Additionally, the references of all full text articles appraised for eligibility were reviewed to ensure all potentially eligible articles were found by the database and national trauma association abstract search.
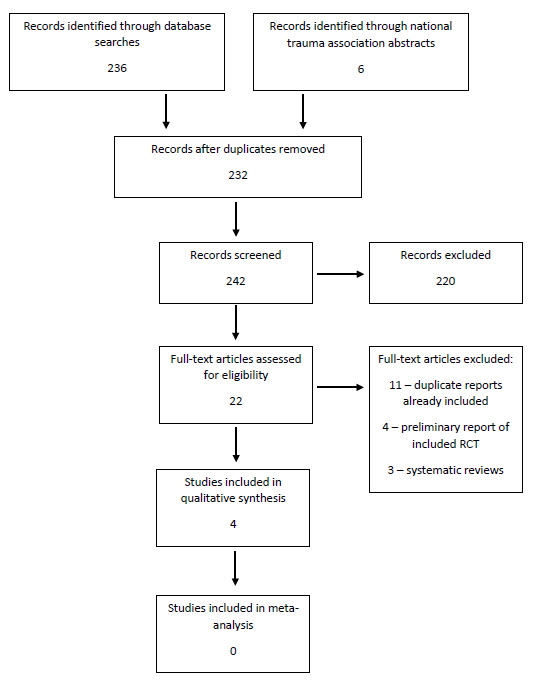
PRISMA Flow Diagram
Appraisal of Chosen Articles/Literature Review:
Randomized Clinical Trials, ordered from oldest to most recent
| Immediate Versus Delayed Resuscitation for Hypotensive Patients with Penetrating Torso Injuries13 Bickell, et al |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PICO Question | Population – hypotensive, adult patients with penetrating torso injuries requiring operative intervention for hemorrhage control Intervention – delayed resuscitation until arrival in operating room Comparison – immediate resuscitation (standard paramedical protocol in field, crystalloid and blood transfusions as indicated based upon established criteria) Outcome – in-hospital mortality, morbidities (wound infection, adult respiratory distress syndrome, sepsis, acute renal failure, coagulopathy, pneumonia) |
|||||||||
| 1a. Randomization | Not randomized. Patients allocated to one of two groups depending on day – patients injured on even days enrolled in immediate resuscitation group and patients injured on odd days enrolled in delayed resuscitation group. Paramedical and surgical staff performed 24 hour shift every three days. Though no reports of patients non-enrollment due to a lack of prehospital allocation concealment were reported, it is unknown if this allocation scheme resulted in bias. | |||||||||
| 1b. Groups | The two groups appeared similar in terms of baseline characteristics, mechanism of injury, and severity of injury. Both groups were of penetrating trauma patients without traumatic brain injury. | |||||||||
| 2a. Treatment | Other than the intervention, the groups were treated similarly. | |||||||||
| 2b. Patient Allocation | Analysis was performed on an intent-to-treat basis. All enrolled patients were accounted for and none were lost to follow-up.
|
|||||||||
| 3. Objective measures and blinding | Mortality is an objective outcome and unlikely to be affected by ascertainment bias. The clinicians were not blinded to the intervention as they were required to provide it. It is unclear if the data collectors were blinded to the group allocation. | |||||||||
| 1. Treatment Effect | Outcome – in-hospital mortality Relative Risk = 0.79 (95% CI 0.63 – 0.99) Absolute Risk Reduction = 0.08 or 8% Relative Risk Reduction = 0.21 or 21% Number Needed to Treat = 13 patients Morbidity – no difference in adult respiratory distress syndrome, sepsis, acute renal failure, or pneumonia was observed. |
|||||||||
| Precision of Outcomes | The outcome is precise given the narrow confidence interval (95% CI 0.63 – 0.99). | |||||||||
| External Validity | The population is representative of urban trauma patients suffering penetrating injuries. Though the immediate resuscitation group received a significantly greater volume of fluid in both the prehospital (870 cc versus 92 cc, p<0.001) and emergency department (1,608 cc versus 283 cc, p<0.001), the differences in systolic blood pressure upon arrival to the operating room was not significantly different (immediate resuscitation 112 mmHg versus delayed resuscitation 113 mmHg, p 0.98). This brings into question the causal relationship between permissive hypotension and mortality; that is, does increasing the blood pressure increase mortality or does large volume crystalloid resuscitation through its deleterious effects increase mortality?
As the complications associated with crystalloid resuscitation have become known, a shift has occurred in which we resuscitate bleeding patients with essentially reconstituted whole blood (high ratios of red blood cells, plasma, and platelets). Given the change in resuscitation from the time this study was performed (1989-1992), this study may lack external validity. Especially if it is the crystalloid and not the lower blood pressure that was the causal agent for decreasing mortality. |
|||||||||
| Hypotensive Resuscitation during Active Hemorrhage: Impact on In-Hospital Mortality 14 Dutton, et al |
|
|---|---|
| PICO Question | Population – adult trauma patients aged <56 (unclear why this cutoff was chosen) with a SBP 70 mmHg Control – resuscitation titrated to goal of SBP >100 mmHg Outcome – in-hospital mortality |
| 1a. Randomization | Method for randomization was not disclosed in manuscript and the risk of bias is unclear. |
| 1b. Groups | The two groups appeared similar in terms of baseline demographics, mechanism of injury, and injury Severity. This study included patients with both blunt and penetrating trauma. Patients with traumatic brain injury were excluded. |
| 2a. Treatment | Other than the intervention, the groups were treated similarly. |
| 2b. Patient Allocation | All enrolled patients were accounted for in the analysis. It is unclear if there any protocol violations and if the analysis was performed on an intent-to-treat basis. |
| 3. Objective measures and blinding | Mortality is an objective outcome. The clinicians were not blinded to the intervention as they were required to provide it. It is unclear if the data collectors were blinded to the group allocation. |
| 1. Treatment Effect | Outcome – in-hospital mortality Relative Risk = 1 (95% CI 0.26-3.80) Absolute Risk Reduction = 0 or 0% Relative Risk Reduction = 0 or 0% Number Needed to Treat = n/a |
| 2. Precision of Outcomes | This is not a precise outcome as there is a wide confidence interval. |
| External Validity | This study may not have external validity. The overall mortality rate in this study is quite low and lower than would be suspected for severely injured trauma patients (as evidenced by their Injury Severity Scores (treatment group 20 ± 12, control 24 ± 14) and low mortality rate. This makes me question whether patients who might most benefit from permissive hypotension were not included. Also, transfusion and fluid volumes are not provided. This study was performed from 1996-1999 and, like the Bickell study, resuscitation protocols were likely very different, with large volumes of crystalloid being administered. |
| A Controlled Resuscitation Strategy is Feasible and Safe in Hypotensive Trauma Patients: Results of a Prospective Randomized Pilot Trial15 Schreiber, et al |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PICO Question | Population – adult trauma patients without evidence of severe traumatic brain injury with prehospital SBP 70 mmHg or palpable radial pulse Control – patients given an initial 2L fluid and then any additional fluid necessary to keep the blood pressure SBP>110mmHg Outcome – 24 hour mortality |
||||||||||||
| 1a. Randomization | The patients were randomized by a central facility. The method for generating a random sequence was not disclosed. Any stratification by center or injury mechanism is unknown. Containers with either 250cc bags of crystalloid (intervention group) or 1L bag of crystalloid were placed on transport vehicles. The canisters were equally weighted so that that allocation could not be determined by prehospital personnel. | ||||||||||||
| 1b. Groups | The groups were similar at the start of the trial. | ||||||||||||
| 2a. Treatment | At each site in this multicenter study, groups were treated equally except for the intervention. That being said, there may have been regional variations that differed between the centers, especially if randomization was not stratified by center. A separate statistical analysis was adjusted for regional site in an attempt to mitigate the effect of regional variations. | ||||||||||||
| 2b. Patient Allocation | All patients were accounted for. The analysis was performed on an intent-to-treat basis. | ||||||||||||
| 3. Objective measures and blinding | Mortality is an objective outcome. The clinicians were not blinded to the intervention as they were required to provide it. It is unclear if the data collectors were blinded to the group allocation. | ||||||||||||
| 1. Treatment Effect |
*pre-specified subgroups Although the authors pre-specified subgroups, they did not stratify by mechanism. They did not check for an interaction between mechanism and controlled resuscitation. Therefore, no conclusion can be made regarding whether there are any differences in the effect of controlled intervention in blunt versus penetrating trauma patients. Further study is necessary. |
||||||||||||
| 2. Precision of Outcomes | The estimate of effect of controlled resuscitation on the primary outcome (24 hour mortality) is moderately precise. The secondary outcome of 30-day mortality is not very precise. The confidence interval for the estimate of effect for the penetrating trauma subgroup analysis for penetrating trauma is wide, likely a result of small numbers. The confidence interval for the estimate for blunt trauma is more precise, but the credibility of the point estimate is diminished by the post-hoc analysis. | ||||||||||||
| External Validity | This study appears to be generalizable as the population is representative and the treatment is feasible. That being said, as in the Bickell et al study, though the intervention group was given much less fluid, admission SBP was not significantly different between the two groups. This study has external validity. | ||||||||||||
| Intraoperative Hypotensive Resuscitation for Patients Undergoing Laparotomy or Thoracotomy for Trauma: Early Termination of a Randomized Prospective Clinical Trial16 Carrick, et al |
|
|---|---|
| PICO Question | Population – adult trauma patients (age <46) with in-hospital SBP 50 mmHg Control – intraoperative resuscitation goal of MAP >65 mmHg Outcome – 30 day mortality |
| 1a. Randomization | Trial was randomized with sealed envelopes prepared by a third party (unknown if consecutively numbered or opaque) at the operating room door. The method of randomization was not disclosed. |
| 1b. Groups | The two groups had similar demographics, physiology upon arrival, and injury severity. Because of an imbalance in the random allocation of blunt trauma patients, blunt mechanism was added to the exclusion criteria and the 9 blunt trauma patients randomized were excluded from the analysis (1 from intervention group and 8 from control group). Additionally, 3 were excluded as they did not undergo the planned operation (2 in the intervention group and 1 in the control group). Four were lost to follow up and not included (2 in the intervention group and 2 in the control group).
The exclusion of blunt and non-operative patients following randomization violates the principle of intention to treat. The intention to treat principle is the most cautious, thereby minimizing Type I error and allows for the greatest external validity. If the treatment to which a patient was randomized then influenced to ultimate decision regarding inclusion, this results in bias in the study and decreases the internal validity. |
| 2a. Treatment | Aside from intervention, both groups were treated with usual care. Of note, this intervention was hospital-based, unlike the Bickell et al study. |
| 2b. Patient Allocation | The study states that the analysis was performed on an intent-to-treat basis, but the exclusion of blunt trauma patients contradicts that statement as they were randomized into the study. One blunt trauma patient was excluded from the intervention group and 8 from the control group. Additionally, 3 patients were randomized but not included as they did not have a laparotomy or thoracotomy. |
| 3. Objective measures and blinding | Mortality is an objective outcome. The clinicians were not blinded to the intervention as they were required to provide it. It is unclear if the data collectors were blinded to the group allocation. |
| 1. Treatment Effect | Outcome – 30 day mortality Relative Risk = 0.82 (95% CI 0.47 – 1.42) Absolute Risk Reduction = 0.05 or 5% Relative Risk Reduction = 0.18 or 18% Number Needed to Treat = 21 |
| 2. Precision of Outcomes | The outcome mortality is not precise given the wide confidence interval. |
| External Validity | The external validity of the study is in question. First, the time frame of the study (2007-2013) occurred over a time period when resuscitation practices changed dramatically across the country. Second, the results of this study only apply to patients with penetrating injuries. |
| Special Note | The trial was stopped early for futility in enrolling the desired sample size. Stopping early can result in a more biased estimate of treatment effect. Additionally, it may increase imbalances in baseline characteristics between the two groups, especially since the method of randomization was not specified (unsure if block or stratified). While no measured baseline variables appear unbalanced on Table 1 of the paper (except for mechanism), unmeasured variables may be different. Stopping for futility may preclude analyses of secondary outcomes. |
Grading of Evidence
- In patients with penetrating trauma, does controlled resuscitation (permissive hypotension) until hemorrhage is controlled decrease in-hospital mortality?There is insufficient evidence that controlled resuscitation (permissive hypotension) results in decreased mortality specifically in patients suffering penetrating injuries. The Bickell study showed a dramatic decrease in mortality but was performed in an era where resuscitation was significantly different. Thus, it no longer has external validity. The Carrick study appears to be at significant risk of bias. In it, controlled resuscitation was not found to be superior to standard resuscitation and, given the wide confidence interval, we cannot be sure that it does not increase 30-day mortality.On the other hand, Schreiber’s paper showed a significant reduction in 24-hour mortality for all trauma patients. Given that there are no other studies with a result consistent with Schreiber’s, that there is not necessarily biologic plausibility to the mechanism of injury being a moderator of treatment effect, and that the subgroup was not specified a priori, the reader cannot be sure that the results of the subgroup analysis are not due to chance alone.17 Although the subgroup analysis for penetrating trauma patients failed to show a similar reduction in mortality, those results could be due to chance alone given the methodologic flaws of the subgroup analysis. Thus, we are left with the results of Schreiber’s paper for to state that there is moderate certainty of a substantial benefit to the use-controlled resuscitation in all patients (RRR 65%, NNT 11).Recommendation: Controlled resuscitation (permissive hypotension) should be used in patients with penetrating trauma
Level of Evidence: Moderate
Net Benefit: Substantial
Grade of Recommendation: B (intervention recommended – there is moderate certainty that the net benefit is substantial) - In patients with blunt trauma, does controlled resuscitation (permissive hypotension) until hemorrhage is controlled decrease in-hospital mortality?In patients specifically with blunt trauma, it is unclear if controlled resuscitation (permissive hypotension) results in decreased mortality. Schreiber’s paper is the only included paper to report the outcomes of blunt trauma patients. The strength of the recommendation is limited by the study design. The mechanism subgroup was not specified a priori. The subgroup analysis for patients suffering blunt trauma is methodologically flawed, as is the subgroup analysis for penetrating trauma patients. Thus, we are left with the results of Schreiber’s paper for to state that there is moderate certainty of a substantial benefit to the use-controlled resuscitation in all patients (RRR 65%, NNT 11).Recommendation: Controlled resuscitation (permissive hypotension) should be used in blunt trauma patients without traumatic brain injury
Level of Evidence: Moderate
Net Benefit: Substantial
Grade of Recommendation: B (intervention recommended – there is moderate certainty that the net benefit is moderate to substantial)
Summary of Recommendations/Guideline
For hypotensive patients arriving to the trauma center with penetrating or blunt trauma, resuscitation should be titrated to a systolic blood pressure >70 mmHg until ongoing hemorrhage has been ruled out or control of hemorrhage has been obtained.
References:
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Injury Prevention and Control [online]. Accessed September 20, 2015.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web–based Injury Statistics Query and Reporting System (WISQARS) [online]. Accessed September 20, 2015.
- Tisherman SA, Schmicker RH, Brasel KJ, Bulger EM, Kerby JD, Minei JP, Powell JL, Reiff DA, Rizoli SB, Schreiber MA. Detailed Description of All Deaths in Both the Shock and Traumatic Brain Injury Hypertonic Saline Trials of the Resuscitation Outcomes Consortium. Ann Surg. Mar 2015;261(3):586-90.
- Davis JS, Satahoo SS, Butler FK, Dermer H, Naranjo D, Julien K, Van Haren RM, Namias N, Blackbourne LH, Schulman CL. An Analysis of Prehospital Deaths: Who Can we Save? J Trauma Acute Care Surg. 77(2):213-18.
- Shackford DR, Mackersie RC, Hoyt DB, Baxt WG, Eastman AB, Hammill FN, Knotts FB, Virgilio RW. Impact of a Trauma System on Outcome of Severely Injured Patients. Arch Surg. May 1987;122(5):523-27.
- Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to Laparotomy for Intra-Abdominal Bleeding from Trauma Does Affect Survival for Delays up to 90 Minutes. J Trauma. March 2002;52(3):420-25.
- Johansson PI, Oliveri RS, Ostrowski SR. Hemostatic Resuscitation with Plasma and Platelets in Trauma. J Emerg Trauma Shock. Apr-Jun 2012;5(2):120-25.
- Kisat M, Morrison JJ, Hashmi ZG, Efron DT, Rasmussen TE, Haider AH. Epidemiology and Outcomes of Non-Compressible Torso Hemorrhage. J Surg Res. 2013;184(1):414-21.
- Shires T, Coln D, Carrico J, Lightfoot S. Fluid Therapy in Hemorrhagic Shock. Arch Surg. Apr 1964;88:688-93.
- Bickell WH, Bruttig SP, Millnamow GA, O’Benar J, Wade CE. The Detrimental Effects of Intravenous Crystalloid after Aortotomy in Swine. Surgery. Sep 1991;110(3):529-36.
- Stern SA, Dronen SC, Birrer P, Wang X. Effect of Blood Pressure on Hemorrhage Volume and Survival in a Near-Fatal Hemorrhage Model Incorporating a Vascular Injury. Ann Emerg Med. Feb 1993;22(2):155-63.
- Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D, Methods Work Group, Third US Preventive Services Task Force. Current Methods of the US Preventive Services Task Force: a Review of the Process. Am J Prev Med. Apr 2001;20(3 Suppl):21-25.
- Bickell WH, Wall MJ, Pepe PE, Martin RR, Ginger VF, Allen MK, Mattox KL. Immediate Versus Delayed Fluid Resuscitation for Hypotensive Patients with Penetrating Torso Injuries. NEJM. Oct 1994;331(17):1105-09.
- Dutton RP, Mackenzie CF, Scalea TM. Hypotensive Resuscitation during Active Hemorrhage: Impact on In-Hospital Mortality. J Trauma. June 2002;52(6):1141-46.
- Schreiber MA, Meier EN, Tisherman SA, Kerby JD, Newgard CD, Brasel K, Egan D, Witham W, Williams C, Daya M, Beeson J, McCully BH, Wheeler S, Kannas D, May S, McKnight B, Hoyt DB; ROC Investigators. A Controlled Resuscitation Strategy is Feasible and Safe in Hypotensive Trauma Patients: Results of a Prospective Randomized Pilot Trial. J Trauma Acute Care Surg. Apr 2015;78(4):687-95.
- Carrick MM, Morrison CA, Tapia NM, Leonard J, Suliburk JW, Norman MA, Welsh FJ, Scott BG, Liscum KR, Raty SR, Wall MJ, Mattox KL. Intraoperative Hypotensive Resuscitation for Patients Undergoing Laparotomy or Thoracotomy for Trauma: Early Termination of a Randomized Prospective Clinical Trial. J Trauma Acute Care Surg. Jun 2016;80(6):886-96.
- Sun X, Ioannidis JP, Agoritsas T, Alba AC, Guyatt G. How to Use a Subgroup Analysis. JAMA. Jan 2014;311(4):405-11.