Students – Still in Training

Pexels: Hawk ii
Students in training play an important role in everyday medical work. They help gather information, support documentation, and assist with patient care tasks that keep clinics and hospitals running smoothly. Their involvement gives organizations added support while giving students the hands‑on experience they need to grow into confident, capable clinicians.
Because students contribute meaningfully to patient care, it’s important to understand how to use them safely and compliantly. This includes knowing what they are allowed to do, how their documentation can be used, and what level of supervision is required. With clear expectations and proper oversight, students can strengthen team workflows while maintaining full compliance with CMS, Novitas, and Texas Medicaid requirements.
CMS/Medicare definitions:
- Medical students are individuals enrolled in an accredited medical/health professions school, not in a GME (residency) program.
- APP students (NP, PA, CNS, CNM students) follow similar rules — they are not licensed practitioners and cannot independently bill or perform services.
- Therapy students (PT/OT/SLP) must follow state scope, board requirements, and CMS therapy student rules, which differ significantly from MD/NP/PA student rules.
Medicare never reimburses for student work but allows teaching providers to verify and use student documentation under strict conditions. So, what can they contribute?
CMS / Medicare Rules for Student Documentation2
- Evaluation & Management (E/M) Services
CMS permits teaching physicians (and some APP preceptors) to use student documentation for E/M if:
Requirements
- Teaching Physician is physically present for all student contributions except history-taking.
- Teaching Physician verifies all student documentation (history, exam, MDM).
- Teaching Physician personally performs or re‑performs:
- The physical exam
- The medical decision making
- Student documentation may be used but cannot stand alone.
CMS explicitly states teaching physicians may verify rather than re‑document medical student notes. This reduces burden and is widely used in academic settings.
What Students May Document2
- History, ROS, PFSH
- Exam (but TP must re‑perform)
- Medical decision making (but TP must re‑perform)
- Procedures: never billable based on student work
Billing
- Payment is based on provider work, not student work.
CPT/AMA Guidance
The AMA confirms:
- Teaching physicians may verify student entries rather than re‑documenting them (E/M only).
- Verification requires signature + date and re‑performance of exam and MDM.
- Students cannot independently perform billable procedures but may assist.
Novitas (MAC JH – Texas) Requirements
- Student participation must occur in the physical presence of the teaching physician (or resident).
- Teaching physician must verify all student documentation.
- Students may document ROS and PFSH independently; TP must review.
- Students cannot independently furnish billable services.
Novitas reiterates that payment is based on teaching physician work, not student work.
Texas Medicaid Requirements
Texas Medicaid does not have its own standalone “student documentation” rule; instead, it generally follows:
- CMS teaching physician rules for MD/DO
- Follow the same rules for NP/PA students as you would medical students
- Reminder: Teaching Physician rules do not apply to Advance Practice Providers, as they are not physicians. The concept of supervision for students may still apply
- State practice act + board requirements for therapy professions (PT/OT/SLP)
Important Texas Medicaid Points
- Texas Medicaid requires that the billing provider meet all documentation, supervision, and medical necessity rules.
- Students cannot be considered rendering providers.
- APP students may not function as “incident‑to” extenders.
Therapy Students (PT / OT / SLP)
CMS Therapy Student Rule:
- Students may participate in therapy services.
- For Medicare Part B:
- Only the licensed therapist’s time counts toward billable minutes.
- Student time does NOT count unless the therapist is directing the service and is not engaged with another patient.
- Documentation must clearly show the licensed therapist’s active involvement.
Though CMS Article A53339 has been retired and does not point to an LCD policy doesn’t mean that the information contained in it aren’t relative. With lack of other guidance, it is still a best practice resource.
Allowed Uses of Students (Across Professions)
Students May:
- Take history, ROS, PFSH
- Perform physical exam (TP must re‑perform)
- Document findings in the medical record
- Assist in procedures under direct supervision
- Contribute to care coordination
- Enhance throughput in teaching practices
- Help reduce documentation burden when compliance rules are followed
Students May Not:
- Independently perform billable services
- Contribute to diagnostic/therapeutic procedures without direct supervision
- Establish medical necessity
- Act as the rendering provider
- Generate billable minutes (therapy except under strict conditions)
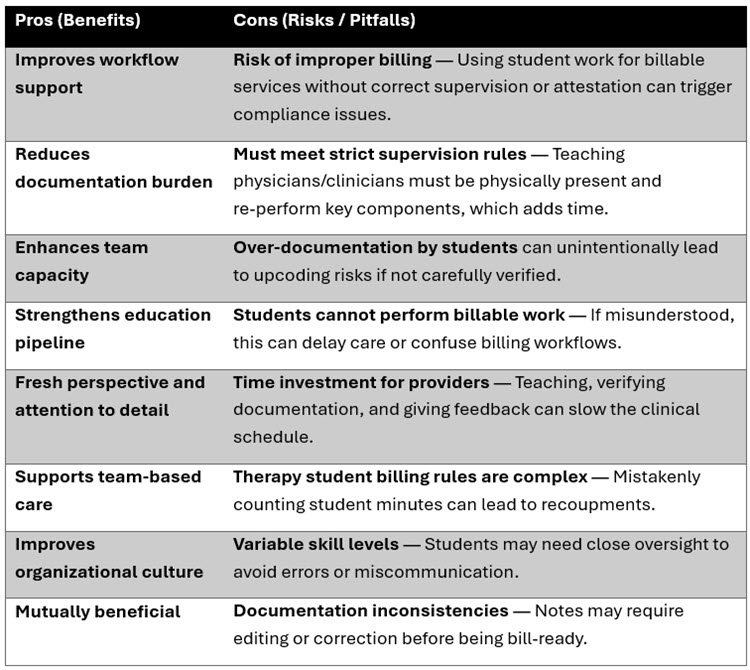
Pros vs. Cons of Using Students in Clinical Care
Final Thoughts
With thoughtful oversight and adherence to compliance standards, involving students in clinical care enhances both organizational efficiency and student learning.
Resources
UT Health Medical School Policy 400.0 (Internal Link)
Bethel University PA Program: CMS Guidelines for Student Work (Preceptor Guidelines)