Team Documentation
What is Team Documentation?
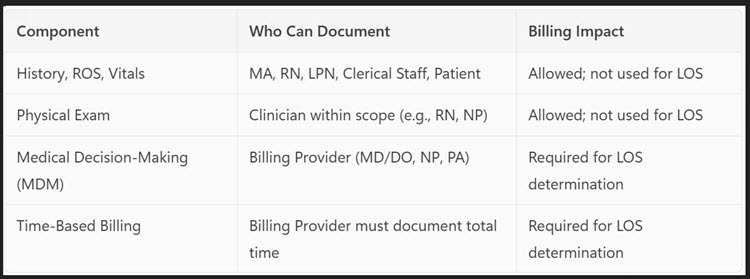
Team Documentation—also known as multiple contributor documentation—is a collaborative approach where non-physician team members assist with documenting patient visits, entering orders, reconciling medications, and preparing prescriptions. These contributors can include:
- Clinical staff: Medical Assistants (MAs), Licensed Practical Nurses (LPNs), Registered Nurses (RNs), Advanced Practice Clinicians (APCs)
- Nonclinical staff: Scribes, transcriptionists, students
- Patients: In some EHR systems, patients can input parts of their history or medication lists
Who can document what?
Split/Shared Facility Setting
A split/shared visit is an E/M service performed jointly by a physician and a non-physician practitioner (APP) (e.g., NP, CNS, or PA) in a facility setting.
Substantive Portion Rule (2024 Update)
- The billing provider must perform more than half of the total time or the substantive part of the MDM.
- Team documentation can support the visit, but:
- Each provider must document their own contributions.
- A generic attestation (e.g., “I agree with the plan”) is not sufficient.
Teaching Setting
- Team members (e.g., residents, nurses, MAs) can document portions of the visit (e.g., history, ROS, vitals).
- Teaching physicians may rely on this documentation if they:
- Are physically present during the key portions of the service.
- Sign and date the note to affirm their participation and oversight.
Attestation Requirements
- The teaching physician must document:
- Their presence and personal involvement in the care.
- Any changes to the plan of care.
- Their agreement or disagreement with the resident’s findings.
- Team documentation can support the note, but only the teaching physician can bill, and they must verify and supplement the documentation as needed.
Team Documentation vs. Scribe Services
A scribe has no clinical input in the patient encounter except to transcribe the exact words of the provider performing the service. They may not impart any clinical observation or perform any clinical tasks. They are a transcription service.
Why is this distinction important?
Understanding the distinction between a scribe and a team member contributing to documentation is crucial for maintaining compliance, billing accuracy, and clinical integrity in a medical setting.
1. Legal and Regulatory Compliance
- Scribes are typically not licensed clinicians and are only permitted to transcribe what the provider says during the encounter.
- Team members (e.g., nurses, MAs, APCs) may document independent observations or actions within their scope of practice.
- Mislabeling a team member as a scribe—or vice versa—can lead to CMS violations, audit failures, or fraudulent billing.
2. Billing and Reimbursement Accuracy
- Scribe documentation must be affirmed by the provider (e.g., “I have reviewed and agree with the above note”).
- Team documentation must be authenticated by each contributor, and the billing provider must document the MDM or time for E/M services.
- Incorrect attribution can result in denied claims or overpayments, triggering audits or paybacks.
3. Scope of Practice and Role Clarity
- Scribes do not perform clinical tasks or make decisions.
- Team members may:
- Take vitals
- Reconcile medications
- Document history
- Perform portions of the physical exam (if licensed)
- Confusing these roles can lead to scope-of-practice violations or patient safety risks.
4. Audit Readiness and Documentation Integrity
- Auditors look for:
- Who documented what.
- Whether documentation supports billed services.
- Proper authentication and attestation.
- Clear role delineation ensures that documentation is defensible, complete, and compliant.
5. Training and Workflow Optimization
- Understanding the distinction helps:
- Assign tasks appropriately
- Train staff effectively
- Reduce provider burnout
- Improve team-based care delivery
Team Documentation in Healthcare: A Smarter, Safer Way to Share the Chart
Team Documentation is a collaborative approach to clinical charting where multiple healthcare team members—such as nurses, medical assistants, and even patients—contribute to the medical record. Unlike traditional scribing, where a person transcribes a provider’s words in real time, team documentation allows each contributor to document tasks they personally perform, all within their scope of practice.
This model improves efficiency, reduces provider burnout, and enhances patient care by distributing documentation responsibilities across the care team. However, it must be implemented with clear role definitions, proper training, and strict adherence to CMS, CPT, and Novitas guidelines.
When done right, team documentation supports a more connected, compliant, and patient-centered care environment.
Resources: