Understanding Your Taxonomy Designation
What is a taxonomy code?
The taxonomy code is a 10-character code that is self-selected by the physician that best describes their education and specialty training. They must designate a primary taxonomy but may also select any subspecialties they are trained for. It is important to make sure these are correctly assigned as they are tied to the provider’s NPI (National Provider Identifier). If the incorrect taxonomy is assigned to their NPI, this may cause concurrent care billing issues with their colleagues.
What is the NUCC?
The NUCC (National Uniform Claim Committee) taxonomy codes are a standardized set of alphanumeric codes used to classify healthcare providers by:
- Provider Grouping (e.g., Allopathic & Osteopathic Physicians)
- Classification (e.g., Internal Medicine)
- Area of Specialization (e.g., Critical Care Medicine)
These codes do not define the services rendered but rather the provider’s role and/or specialty. The NUCC is where you find taxonomy codes. These codes are updated twice a year.
How Taxonomy Codes Apply to Concurrent Care
Concurrent care refers to situations where multiple providers are delivering similar or overlapping services to the same patient at the same time—often seen in complex cases like palliative care, chronic disease management, or behavioral health.
How to apply taxonomy codes effectively in concurrent care:
- Differentiate Provider Roles:
- Use distinct taxonomy codes to reflect each provider’s unique role.
- For example, a Primary Care Physician (PCP) might use 207Q00000X (Family Medicine), while a Palliative Care Specialist might use 208D00000X (Hospice and Palliative Medicine).
- Support Medical Necessity:
- Proper taxonomy coding helps justify why multiple providers are involved.
- It shows that each provider brings a different specialty or perspective to the patient’s care.
- Avoid Claim Denials:
- Payers often scrutinize concurrent care claims.
- Using accurate taxonomy codes helps demonstrate that services are not duplicative.
- Document clearly in the patient’s record how each provider’s role is distinct and necessary.
- Coordinate with NPI:
- Each provider’s NPI must be associated with the correct taxonomy code(s).
- One taxonomy code must be marked as primary when applying for or updating an NPI.
Concurrent Critical Care Example:
ICU patient is being managed by both a Pulmonary Critical Care specialist and a Cardiologist.
Pulmonary Critical Care Note:
Provider: Dr. Jane Smith, MD
Taxonomy: 207RC0200X (Pulmonary Critical Care)
Date/Time: 06/26/2025, 08:00 AM
Chief Concern: Acute hypoxic respiratory failure secondary to pneumonia.
Assessment/Plan:
Initiated mechanical ventilation with lung-protective strategy. Adjusted ventilator settings based on ABG and compliance. Managed sedation and neuromuscular blockade and coordinated with ID for antibiotic coverage.
Time Spent: 60 minutes of critical care time.
——————————————————————————————————————
Cardiologist Dr. John Doe is concurrently managing cardiac arrhythmia and hemodynamic instability. No duplication of services.
Cardiology Note:
Provider: Dr. John Doe, MD
Taxonomy: 207RC0000X (Cardiology)
Date/Time: 06/26/2025, 08:30 AM
Chief Concern: New-onset atrial fibrillation with RVR in the setting of sepsis.
Assessment/Plan:
Started IV amiodarone and rate control strategy. Observed for QT prolongation and electrolyte imbalances and collaborated with the ICU team for hemodynamic support.
Time Spent: 40 minutes of critical care time.
Note: Care provided is distinct from pulmonary management. No overlap in services
Each of these providers may see the patient on the same day for distinct anatomical and clinical issues.
How CMS Uses Taxonomy Codes in Claim Review
Historically, Medicare did not fully acknowledge all physician subspecialties in contexts such as concurrent care, new patient evaluations, and critical care. However, the system has since evolved and now possesses a greater capacity to identify and differentiate these self-reported subspecialties.
While the primary taxonomy code is the default classification used for most administrative purposes, CMS systems can access all taxonomy codes associated with a provider’s NPI when evaluating:
- Eligibility for new patient visits
- Concurrent care billing
- Specialty-specific services
This means that subspecialty taxonomy codes can be used to differentiate provider roles—if they are properly registered in NPPES and used consistently in claims. That said, concurrent care many times boils down to the primary taxonomy assigned as the Medicare Specialty Code.
What are Medicare Specialty Codes?
Medicare specialty codes are numeric identifiers used by CMS to designate a provider’s primary specialty for purposes such as billing, claims processing, and utilization tracking. These codes are limited in number, and not all medical subspecialties are individually represented. In Medicare claims, specialty codes play a key role in determining payment rules, coverage policies, and service eligibility. While providers can designate both a primary and secondary specialty, typically only one is used for billing, depending on system capabilities.
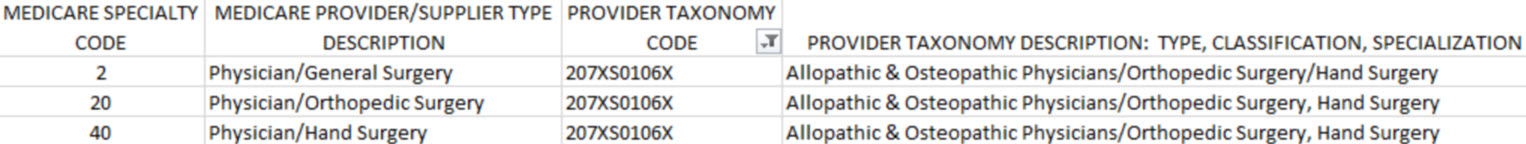
For example:
The taxonomy designation is important, but the Medicare Specialty Code is just as important.
Coding and Billing Tips:
- Credentialing: Ensure each provider is registered with the correct taxonomy in NPPES and Medicare PECOS.
- Documentation:
- Clearly define each provider’s role.
- This also pertains to co-surgery and other procedures, not just E/M services.
- Avoid overlap in history, exam, and decision-making (copy/paste, cloning, etc.)
- Billing:
- Use appropriate modifiers (e.g., 25 for separate E/M on the same day).
- For critical care, document time spent and medical necessity.
Best Practices for Clear Documentation
- Use specific language (e.g., “managed ventilator settings” vs. “followed patient”).
- Include time-based services (e.g., “45 minutes of critical care provided”).
- Reference other providers involved and clarify roles.
- Align documentation with taxonomy code and clinical specialty.
Providers self-select their taxonomy codes based on their education, training, and the nature of the services they offer. These codes are not intended to define the specific services rendered, but rather to reflect the provider’s role or area of specialization. The Medicare Specialty Code points to the primary taxonomy code assigned and is typically the one Medicare uses for coding and billing issues.
This distinction is crucial in understanding how your specialty or subspecialty informs your approach to caring for a patient who may also be under the care of your colleagues—thereby helping to prevent issues related to concurrent care.
Resources
2025 Medicare Provider Crosswalk
Medicare Claims Processing Manual: 10.8 Requirements for Specialty Codes
Data.CMS.gov – Understanding the Data
NPPES – National Provider & Provider Enumeration System