Remote Patient Monitoring (RPM)

Image: Pexels/Pavel Danilyuk
New RPM Code Changes Effective January 1, 2026
The AMA has expanded the Remote Patient Monitoring (RPM) code set by adding new time‑based options for shorter monitoring periods and lighter management.
Why the change?
Previously, RPM billing required:
- Device supply: ≥16 days of data in a 30‑day period
- Management time: ≥20 minutes per month
These thresholds didn’t fit common scenarios like 10–14 days post‑discharge monitoring or brief monthly check‑ins.
New 2026 Codes:
99445 — Device supply for 2–15 days
Use for short‑term monitoring (e.g., post‑discharge, medication titration).
Compliance Tip: Bill once per 30 days; choose 99445 OR 99454, not both.
99470 — Treatment management, first 10 minutes
Use when monthly management time is 10–19 minutes.
Compliance Tip: If time reaches ≥20 minutes, use 99457 instead. 99470 and 99457 cannot be billed together.
Existing Codes:
- 99453 — Initial setup and patient education
- 99454 — Device supply for 16–30 days
- 99457 — Treatment management, first 20 minutes
- +99458 — Each additional 20 minutes
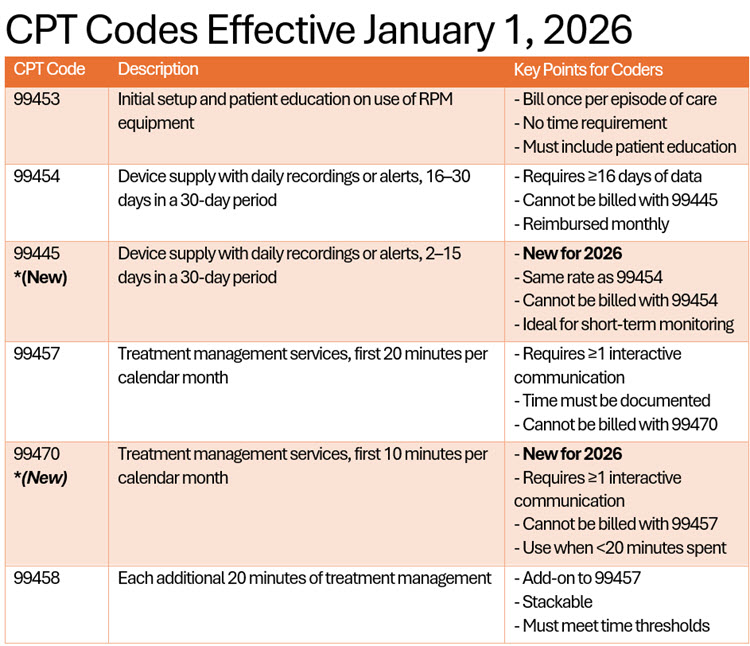
Quick Reference Table
Key Coding Tips for New RPM Coders:
-
- Time and Data Thresholds Matter:
- Use 99454 for ≥16 days of data.
- Use 99445 for 2–15 days of data.
- Use 99457 for ≥20 minutes of management.
- Use 99470 for 10–19 minutes of management.
- Codes Are Not Additive:
- Do not bill 99445 and 99454 together.
- Do not bill 99470 and 99457 together.
- Interactive Communication Required:
- For 99457 and 99470, at least one real-time interaction (audio/video or secure messaging) is required.
- Documentation Must Support:
- Device setup, patient education, data transmission days, and time spent must be clearly documented.
- Billing Frequency:
- RPM codes are billed monthly, not per encounter.
- Time and Data Thresholds Matter:
Remote Patient Monitoring (RPM) is under heightened scrutiny by federal and state oversight bodies, including CMS, OIG, DOJ, and Medicaid Program Integrity units. These agencies are actively auditing RPM claims to verify medical necessity, proper coding, and accurate billing. Noncompliance can trigger repayment demands, civil penalties, and even fraud investigations.
Resources:
- AMA CPT® 2026 press announcement (digital health & shorter‑duration remote monitoring highlighted):
AMA releases CPT 2026 code set - Professional coding summary of RPM changes (descriptors and family changes):
AAPC: CPT® 2026—The Wait Is Over - CMS PFS final rule and implementation explainers (programmatic framing):
Rimidi: CMS Finalizes RPM Code Expansion in 2026 | Vivo Care: New RPM Codes 99445 & 99470 - Policy/legal commentary on lowering thresholds (background & intent):
McDonald Hopkins: CMS proposes lower time thresholds - CMS Remote Patient Monitoring | CMS