Remote Therapeutic Monitoring (RTM)
What is RTM?
CMS pays for remote monitoring of non‑physiologic data tied to a therapeutic plan (e.g., therapy adherence, pain/function response, MSK/respiratory status, digital therapeutic engagement). RTM data may be patient‑reported using an FDA‑defined medical device (or software as a medical device) and can support rehab, pulmonary, and digital therapeutics programs.
Not to be confused with RPM. RPM (Remote Patient Monitoring) requires automatic physiologic capture and is distinct from RTM; both cannot be billed together by the same practitioner for the same period.
RTM Coding in 3 Easy Steps!
Step 1 — Initial set-up (98975)
- This may only be reported once per episode of care.
- 98975 may not be reported again until the targeted treatment goals have been reached, and a new treatment order is initiated.
Step 2 — Determine Device‑Monitoring Days (30‑Day Period)
2–15 monitored days →
• 98984 (Respiratory)
• 98985 (MSK)
16–30 monitored days → Use “legacy” device codes:
• 98976 – Respiratory
• 98977 – Musculoskeletal
• 98978 – Cognitive Behavioral Therapy (CBT)
Step 3 — Determine Monthly Treatment‑Management Time
10–19 minutes:
• 98979 (must include ≥1 real‑time, synchronous interaction)
≥20 minutes:
• 98980 – Base code (requires ≥1 real‑time interaction)
• 98981 – Add for each additional 20 minutes
Note: The midpoint rule does not apply. Minimum time requirements must be fully met.
Apply Key Billing Rules
- Practitioners must obtain consent either in advance or at the time RTM services are furnished and document that consent in the patient’s record.
- Only one device code per 30‑day period per practitioner.
- Do not bill 98979 and 98980 in the same month.
- Choose either the 2–15‑day family or the 16–30‑day family—not both.
- RTM and RPM cannot be billed together by the same practitioner within the same 30‑day period.
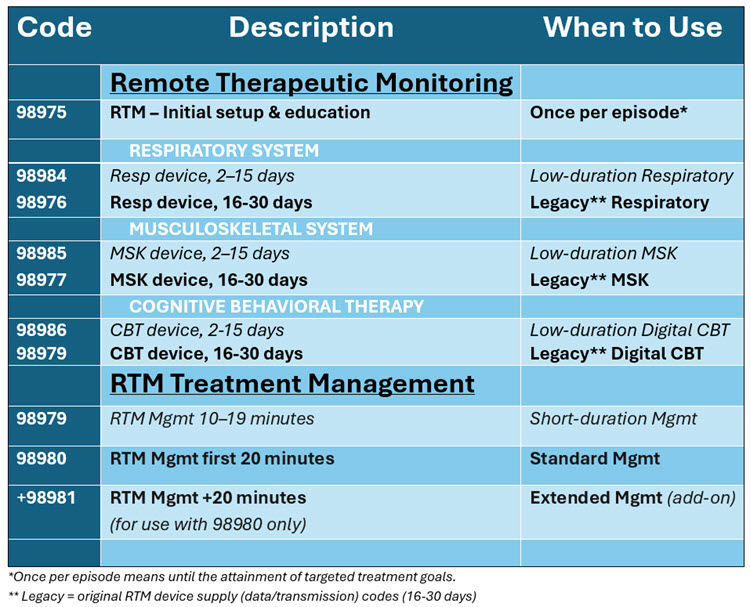
At-a-Glance Coding Table
RTM Coding Examples
1) 98975 – RTM Initial Setup & Patient Education
Scenario: A 58‑year‑old with chronic low back pain begins MSK RTM using an FDA‑defined sensor + app. Clinician provides 12 minutes of onboarding. Documentation: RTM initiated for MSK condition. Device/app education completed. Episode start date noted.
2) 98984 – Respiratory Device Supply (2–15 Days)
Scenario: Asthma patient completes 9 days of inhaler‑sensor monitoring. Documentation: Respiratory device used 9 days.
3) 98985 – MSK Device Supply (2–15 Days)
Scenario: Post‑op meniscus repair patient logs 12 days of MSK sensor‑based rehab. Documentation: MSK device 12 days; 98985 applied.
4) 98976 – Respiratory Device Supply (16–30 Days)
Scenario: COPD patient completes 23 days of monitored respiratory adherence. Documentation: Respiratory RTM device 23 days → 98976.
5) 98977 – MSK Device Supply (16–30 Days)
Scenario: Rotator cuff tear rehab patient logs 21 days of monitored exercises. Documentation: MSK RTM 21 days; 98977 billed.
6) 98978 – CBT Device Supply (16–30 Days)
Scenario: Insomnia patient uses CBT‑I digital therapeutic for 18 days. Documentation: CBT RTM 18 days; 98978 applied.
7) 98979 – RTM Treatment‑Management (10–19 Minutes)
Scenario: ACL‑repair patient: 7 min data review + 5 min plan adjustment + 4 min real‑time call = 16 minutes. Documentation: 16 min RTM management; real‑time call completed.
8) 98980 – RTM Treatment‑Management (First 20 Minutes)
Scenario: Pulmonary patient: 10 min data review + 6 min plan update + 7 min video call = 23 minutes. Documentation: 23 min RTM management with video interaction; 98980 billed.
9) +98981 – RTM Treatment‑Management (Each Additional 20 Minutes)
Scenario: Spine‑surgery patient needs extended management: 45 minutes total.
Code: 98980 + 98981
Documentation: 45 min RTM management; codes 98980 + 98981.
While CMS reimburses RTM and has added these codes as “sometimes therapy,” Texas Medicaid is currently not reimbursing RTM CPT codes. They do, however, reimburse home telemonitoring (RPM) under very specific circumstances.
Resources:
CMS: 2026 CMS Therapy Code List
CMS: Telehealth and Remote Monitoring
CCHP: Patient Telemonitoring