Initial Inpatient or Observation Care Services – Medicare

CMS published their final rule the first week of November. In it, are many direct conflicts with what the AMA’s CPT is publishing for January 1, 2023.
Observation Care Services
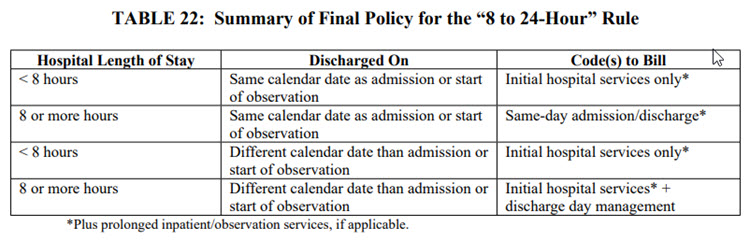
First, let’s discuss the CMS take on the CPT change for Observation Care services. Although Observation will share the same code set with Initial Inpatient Hospital services, the old rules for Observation still apply for Medicare patients. Please see table below for requirements.
CMS PFS (Physician Fee Schedule) Final Rule CY23, pg. 513
b. “8 to 24-Hour Rule” for Hospital Inpatient or Observation Care (pg. 520)
- Please see our related article: CMS FY 2023 Final Rule Changes – Prolonged Services
- CMS – Observation Codes are only for admitting service, specialist use E/M Codes – per Chapter 12 of the Medicare Claims Processing Manual (IOM 100-04), section 30.6.8.A
- *CMS – AI modifier – No changes at this time
- CMS still has the “8 to 24-Hour” rule in place
- Less than 8 hours = 99221-99223 code only
- 8 hours but less than 24 hours – Admit/DC Codes 99234-99236
- Admitted and then discharged after 24 hours – 99221-99223, and 99238-99239 (admission and discharge occurring on separate dates within 24 hours)
- Transition from OBS to Initial Inpatient Hospital stay is still same hospital stay.
- For example: Patient is admitted as an OBS patient. Next day, they are admitted as an Inpatient.
- Coding: Day (1) 99221-99223, Day (2) 99231-99233.
- CMS only allows “attending physician” responsible for discharge to bill 99238, 99239
- CMS does not allow prolonged services with 99238 (30” or less)or 99239 (31” or more)
January 2023 Clarification: Although CPT combined Inpatient Care and Observation Service codes, the original place of service still stands:
- Inpatient Services: (POS 21)
- Observation Services: (POS 22)
Transition from OBS to Inpatient
- CMS/CPT – Transition from OBS to Inpatient: a transition from observation status to inpatient status does not constitute a new stay (Medicare Claims Processing Manual, IOM 100-04, Chapter 12, section 30.6.8.D). For instance, if a practitioner places a beneficiary in observation status on one date of service (and bills an initial observation visit to be described under CPT code 99221 through 99223), and then determines later in the stay that the beneficiary should be admitted to the hospital as an inpatient, the practitioner would not bill a second initial visit for the hospital inpatient stay. Rather, the practitioner would bill the work done on the inpatient admission day as a subsequent visit (CPT codes 99231, 99232, or 99233). This policy aligns with language in the 2023 CPT Codebook instructions. (2023 CPT Codebook, p. 16).
Services performed in other sites on same day of hospital admission
- CMS – Is retaining their original policy that all services from other sites on the date of admission (OBS or IP) are included in the admission code when performed on THE SAME DATE. When services are performed in different sites (even if less than 24 hours has lapsed) you can report E/M (eg, office visit) on day one, and initial hospital code (OBS or IP) on day two. See (Medicare Claims Processing Manual, IOM 100-04, Chapter 12, section 30.6.9.1.A).
- Example A: If a practitioner sees a beneficiary in an office setting at 5 p.m. on April 1st, and the practitioner then admits the beneficiary to the hospital at 7 a.m. on April 2nd, these would be separately billable payments, because initial hospital inpatient or observation care codes (CPT code 99221 through 99223) billed for April 2nd would not retroactively cover the work furnished on April 1st.
- Example B: If the practitioner sees the beneficiary in the office setting at 7 a.m. on April 1st and then admits the beneficiary at 9 p.m. on April 1st, all time the practitioner spent furnishing services to that beneficiary would be reportable under the initial hospital inpatient or observation care code (CPT code 99221 through 99223).
- Example C: If a practitioner may bill only for an initial hospital or observation care service if the practitioner sees a patient in the ED and decides to either place the patient in observation status or admit the patient as a hospital inpatient. For discussion of additional policy proposals regarding patients seen in both the ED and the hospital, refer to section II.F.5. on Emergency Department Services.
- Example D: However, the practitioner can report prolonged inpatient or observation services, as applicable, if time is used to select visit level.
- Please see our related article: CMS FY 2023 Final Rule Changes – Prolonged Services
CMS Definitions
- CMS Definitions – “As we (CMS) do not recognize subspecialties, we proposed slightly amended definitions of “initial” and “subsequent” service”:
- Initial – An initial service would be defined as one that occurs when the patient has not received any professional services from the physician or other qualified health care professional or another physician or other qualified health care professional of the same specialty who belongs to the same group practice during the stay.
- Subsequent – A subsequent service would be defined as one that occurs when the patient has received any professional services from the physician or other qualified health care professional or another physician or other qualified health care professional of the same specialty who belongs to the same group practice during the stay.
Shared/Split Changes
- CMS – Split/Shared rules are as they were for 2022
- Substantive portion may be demonstrated by:
- Documentation of one of the three key components (history, exam, MDM) in its entirety, or
- More than half of the total time (only option for Critical Care Services
- CodingIntel has published a wonderful tool for determining the substantive portion.
- Substantive portion may be demonstrated by:
Critical Care Clarification
- CMS/CPT – Both agree with how “continuous” services that cross midnight are to be counted (AMA pg. 23)
- Critical Care Codes were clarified that ED services and CC services may be performed and reported as long as the ED E/M occurred prior to the Critical Care services by same physician (or physician of same specialty/group practice) and did not require critical care services at that time.
- CMS requires the FULL time in the code descriptor to have been met, not just the mid-point.
- CMS corrected an error in 86 FR 65162 to say that you may not use 99292 until 104”, not 75”, have been met.
- CMS also allows time spent face-to-face on the day of discharge and non-face-to-face services up to 3 days s/p discharge.
If you would like additional training for your group, please reach out to [email protected].