Series Part VI: Chronic Pain Management Services
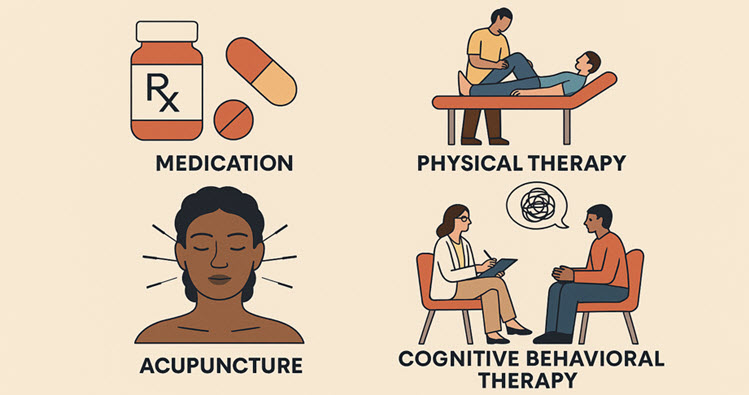
Image Credit: Copilot
The CMS Chronic Pain Management Program was developed in response to the opioid crisis.
In 2018, Congress passed the SUPPORT for Patients and Communities Act, which directed the Centers for Medicare & Medicaid Services (CMS) to create an action plan. The goal was to help prevent opioid addiction by expanding access to medication-assisted treatment (MAT) and promoting non-opioid pain management strategies.
Examples of non-pharmacologic and integrative pain management options, including:
- Electrical nerve stimulation
- Spinal cord stimulation
- Lumbar epidural injections
- Facet joint injections
- Physical and occupational therapy
- Psychiatric and psychological services
- Supervised exercise therapy
- Inpatient and outpatient pain rehabilitation programs
Initial Visit (not separately reimbursable – included in CPM)
Chronic pain management services begin with an in-person, face-to-face visit, conducted by a physician or an advanced practice provider—such as a nurse practitioner, physician assistant, or clinical nurse specialist. Both the patient and the CPM provider must be located in a clinical setting (not home, or via telehealth) for the initial assessment.
This initial visit is bundled into the monthly G3002 HCPCS code, meaning it is not billed separately as an evaluation and management (E/M) service. Once the initial encounter has taken place, follow-up services may be provided through telemedicine, allowing for greater flexibility and access to care. CPM services may begin immediately after the initiating visit requirements are met.
G3002 – Chronic Pain Management and Treatment, Initial 30 Minutes
Chronic pain management and treatment, monthly bundle includes:
- Diagnosis
- Assessment and monitoring
- Administration of a validated pain rating scale or tool
- Development, implementation, revision, and/or maintenance of a person-centered care plan (including strengths, goals, clinical needs, and desired outcomes)
- Overall treatment management
- Coordination of behavioral health treatment
- Medication management
- Pain and health literacy counseling
- Crisis care related to chronic pain
- Ongoing communication and coordination with other practitioners (e.g., PT, OT, integrative care, community-based services
G3003 – Each Additional 15 Minutes of Chronic Pain Management
Each additional 15 minutes of chronic pain management and treatment by a physician or other qualified health care professional, per calendar month.
Documentation Requirements
G3002 – General Documentation Requirements
- Clearly state diagnosis of chronic pain and its impact on function.
- Document patient consent (initial visit only).
- Use a validated pain assessment tool (e.g., PEG scale, Brief Pain Inventory).
- Include time logs for each service provided (e.g., “20 min pain assessment, 10 min care plan discussion”).
G3003 – General Documentation Requirements
- Additional time beyond initial 30 minutes.
- Specify activities performed (e.g., medication adjustment, behavioral health coordination).
- Time per unit (15 min increments) must be clearly documented.
- Avoid duplication with other services (e.g., E/M, psychotherapy).
Billing Requirements
G3002 Billing Requirements: ($82.68 – Houston)
- Initial face-to-face visit required
- First 30 minutes must be personally provided by a physician or APP
- One unit per calendar month
- Time must be ≥30 minutes
G3003 Billing Requirements: ($30.23 per unit – Houston)
- Must be listed separately in addition to G3002
- Time must be ≥15 minutes per unit
- May be billed multiple times per month if time thresholds are met
- Must be personally provided by the billing provider
- Cannot be billed alone — G3002 must be reported first
Key Goals of the CMS Chronic Pain Management Program
The chronic pain management initiative aims to reduce unnecessary exposure to opioids by encouraging safer, evidence-based alternatives. It promotes a personalized approach to care that integrates multimodal and multidisciplinary strategies tailored to each patient’s needs.
By improving access to non-opioid treatments such as physical therapy, acupuncture, and behavioral health services, the program supports more holistic pain relief options. Additionally, it emphasizes the importance of care coordination and ongoing education for both patients and providers, fostering informed decision-making and continuity of care.
Summary
Chronic pain management involves a range of complex requirements that can be challenging to navigate. This article provides a solid starting point, but it’s important to recognize that there’s much more to explore. To deepen your understanding and stay informed, be sure to take advantage of the additional resources listed below.
Resources:
MSHBC – Acupuncture for Chronic Pain Management
MSHBC – CPM Documentation Checklist (Internal Link Only)
Evaluation and Management Services Guide
Novitas – Acupuncture for Pain Management
Documenting for Medical Necessity
JAMA – CBT via Telehealth
HHS – Pain Management Best Practices Report
Aetna – Chronic Pain Management (and related) Policies
BCBS – Biofeedback for Chronic Pain Management
Cigna – Chronic Pain Management Policy
Humana – Chronic Pain Management (and related) Policies
United Healthcare – Chronic Pain Management Policy