High Medical Decision Making – Part One

Image Credit: Pexels/Kampus Production
High-level Medical Decision Making involves more than the use of key phrases; it should be substantiated by corresponding clinical actions. In Part One of this article series, we are going to take a look at how acute complicated injury vs. poses a threat to life or bodily function E/M definitions apply to clinical documentation.
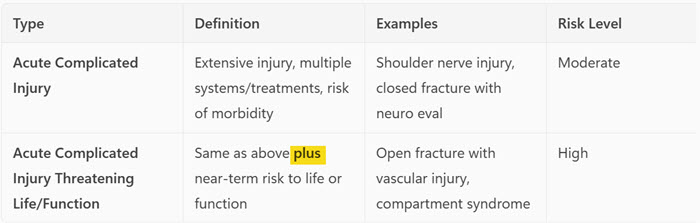
Acute Complicated Injury
The AMA (American Medical Association) defines an acute, complicated injury as “an injury which requires treatment that includes evaluation of body systems that are not directly part of the injured organ, the injury is extensive, or the treatment options are multiple and/or associated with risk of morbidity.”
Acute or chronic illness or injury that poses a threat to life or bodily function:
“An acute illness with systemic symptoms, an acute complicated injury, or a chronic illness or injury with exacerbation and/or progression or side effects of treatment, that poses a threat to life or bodily function in the near term without treatment. Some symptoms may represent a condition that is significantly probable and poses a potential threat to life or bodily function.” These may be included in this category when the evaluation and treatment are consistent with this degree of potential severity.
What does “imminent” or “near term” mean in this context?
Imminent or ‘near term’ implies an immediate or urgent timeframe.
Why does timing matter?
As evidenced above, when documenting a case to support high medical decision-making it is critical to include the appropriate clinical context to accurately reflect the acuity of the patient’s condition. For a diagnosis or condition to qualify as posing a risk to life, significant morbidity, or loss of bodily function, it must meet the threshold of being a near-term threat. This implies that, without timely intervention, the adverse outcome is expected to occur within hours to days—not over weeks, months, or years. The immediacy of the risk should be clearly articulated in the documentation.
Compare and Contrast
Another key point is the distinction between elective and emergent surgical intervention. If documentation indicates that an injury carries a potential risk for morbidity or loss of function, but the procedure is scheduled electively several weeks later, it may not support the criterion of imminent risk. For a condition to meet the threshold of high medical decision-making, the threat to life or function must be immediate—typically requiring intervention within hours to days, not weeks.
Moderate vs. High Medical Decision Making
🔸 Moderate MDM Complexity
Definition: One acute complicated injury or illness with systemic symptoms, or undiagnosed new problem with uncertain prognosis. Moderate risk of morbidity.
Example:
- Partial Rotator Cuff Tear
- Presentation: Shoulder pain with weakness and limited range of motion after a fall. Positive impingement signs.
- Management: Imaging (MRI), referral to orthopedics, possible corticosteroid injection.
- Why Moderate MDM? Acute complicated injury, multiple treatment options, diagnostic uncertainty, moderate risk of functional impairment.
🔺 High MDM Complexity
Definition: One acute or chronic illness or injury that poses a threat to life or bodily function. High risk of morbidity without intervention.
Example:
- Shoulder Dislocation with Neurovascular Compromise
- Presentation: Obvious deformity, absent distal pulses, numbness in the hand after traumatic injury.
- Management: Emergent reduction, vascular imaging, surgical consult.
- Why High MDM? Immediate threat to limb function, urgent intervention required, high risk of permanent disability.
In conclusion, maintaining a clear focus on the principle of medical necessity is essential. Without it, there’s a risk of reducing documentation to a checklist exercise aimed solely at achieving a coding level. The true determinant of medical decision-making lies in the specificity with which we describe the acuity of the problem, the associated risks, and the rationale behind the treatment plan. These elements must be thoughtfully articulated to accurately reflect the complexity of care provided.
Resources
AMA – 2023 E/M Guidelines and Descriptions
AAPC – Determining the level of complexity
NAMAS – Acute Uncomplicated Injury vs. Complicated Injury Article