Prolonged Services

Image: Pexels
Prolonged services are used when a provider spends more time than usual delivering care during an Evaluation and Management (E/M) visit. These services help capture the extra time and complexity involved when a visit goes beyond the typical duration.
Time-Based Billing
When billing for prolonged services, time is the key factor in determining the correct E/M level. This applies when the provider’s total time exceeds the threshold for the highest-level E/M code in that setting.
What Time Can Be Counted?
- Face-to-face time with the patient
- Non-face-to-face time spent on the same day (e.g., reviewing records, documenting, coordinating care)
In some code descriptions—like preventive services—only face-to-face time counts toward prolonged services. Always check the code-specific requirements. Most CPT and HCPCS codes (like +99417, +99418, G2212, G0316–G0318) allow both face-to-face and non-face-to-face time to be counted, as long as it’s performed by the reporting provider on the same date of service.
Key Reminders
- Only one provider’s time can be counted per visit (also see Shared/Split rules).
- Time must be on the same calendar date as the E/M service.
- Documentation must clearly show:
- Total time spent
- That the time exceeded the required threshold
- The medical necessity for the prolonged service
AMA CPT Coding
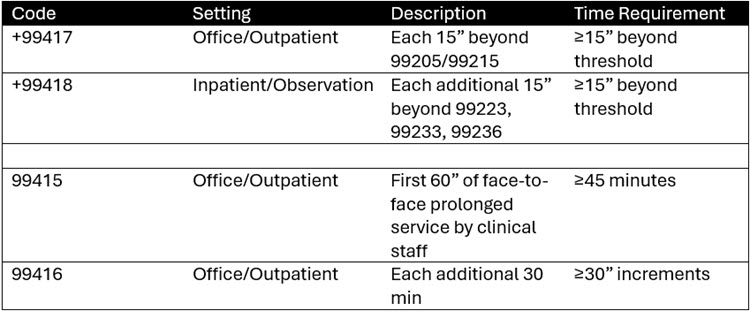
- Time must be personally spent by the reporting provider.
- Includes face-to-face and non-face-to-face time on the same date.
- Cannot be used with psychotherapy codes.
- Midpoint rule does not apply—full 15 minutes must be met.
CMS HCPCS Coding
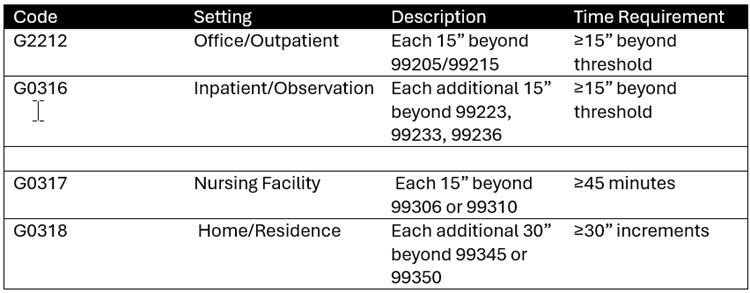
CMS rules differ from CPT:
- CMS requires full value of the primary E/M code to be met plus 15 minutes before prolonged time starts.
- CMS does not recognize CPT codes +99417 and +99418 for Medicare billing.
- CMS includes pre- and post-visit time in some settings (e.g., hospital, nursing facility).
Prolonged Preventive Services
G0513 – Prolonged preventive service(s) (beyond the typical service time of the primary procedure), in the office or other outpatient setting requiring direct patient contact beyond the usual service; first 30 minutes (list separately in addition to code for preventive service)
- Coinsurance and deductible are waived
G0514 -; each additional 30 minutes
- Coinsurance and deductible are waived
Coding Examples
Office or Outpatient Visit – New Patient
Example One: A provider spends 90 minutes on a complex new patient visit.
-
- Clinical Condition: Type 2 DM with poor glycemic control (HbA1c 9.2%)
- CPT billing: 99205 + 99417
- CMS billing: 99205 + G2212 (only if ≥89 minutes)
Office Visit – Established Patient
Example Two: A provider spends 70 minutes managing a chronic condition.
-
- Clinical Condition: Stage 3 CKD (chronic kidney disease)
- CPT billing: 99215 + 99417
- CMS billing: 99215 + G2212
Home or Residence Services
Example Three: A palliative care provider spends 90″ during a home visit coded-99345.
-
- Clinical Condition: Metastatic pancreatic cancer (Stage IV)
- CPT billing: 99345 + 99417
- CMS billing: 99345 + G0318
Inpatient or Observation Services
Example Four: A provider spends 100 minutes on an initial inpatient visit coded as 99236.
-
- Clinical Condition: Acute drug overdose, found unresponsive
- CPT billing: 99236 + 99418
- CMS billing: 99236 + G0316
Cognitive Assessment and Care Planning
Example Five: A provider spends 80 minutes on cognitive assessment.
-
- Clinical Condition: Traumatic brain injury with cognitive sequelae
- CPT billing: 99483 + 99417
- CMS billing: 99483 + G2212
For detailed guidance, please refer to your Medicare contractor’s website to review their specific coverage policies. Keep in mind that CPT and CMS may define time thresholds differently. It’s important to verify which standards your payers follow to ensure accurate reimbursement.
Resources:
CMS MLN Matters: MM12071
CMS PFS: Preventive Services Code List
Noridian Guidance