Getting Started
Safer Culture » INSIDE THE PROJECT » Getting Started
Assess your organizational Safer Culture
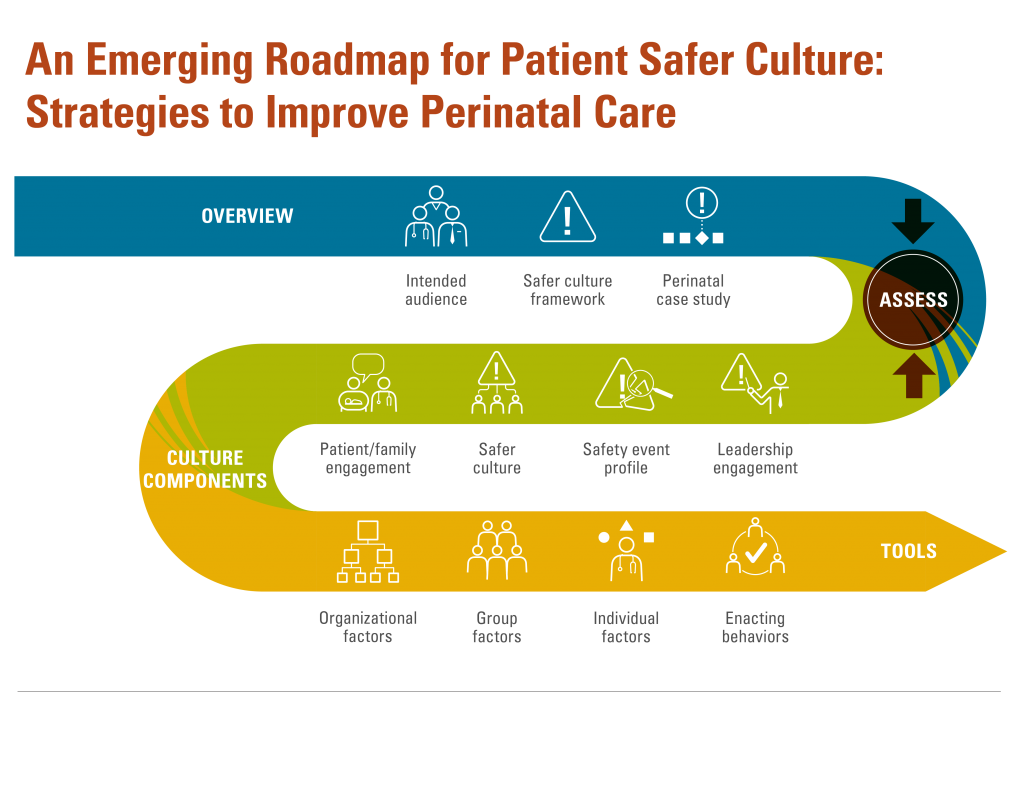
Before you can improve your culture, you have to understand what’s needed and what gaps exist in the healthcare setting. Then you can determine how ready your organization is to address them.
Download the tool: TOOL-Analyzing-Key-Components-Organizational-Safer-Culture
We recommend a four-pronged approach to conducting a Safer Culture needs assessment.
SECURE LEADERSHIP ENGAGEMENT AND COMMITMENT
Ensure leaders are engaged in safety, committed to creating a culture that prioritizes and promotes patient safety, and willing to view patients and families as valuable resources to the team.
Improving the culture of safety requires strong and courageous leaders who “set and demonstrate the behaviors and expectations essential to a safe and transparent culture (Leading a Culture of Safety, ACHE)”. A comprehensive guide for healthcare leaders entitled, “Leading a Culture of Safety: a Blueprint for Success” highlights six leadership domains that require leaders’ attention in building and sustaining a culture of safety:
– Establish a compelling vision of safety
– Value trust, respect, and inclusion
– Select, develop and engage your Board
– Prioritize safety in the selection and development of leaders
– Lead and reward a just culture
– Establish organizational behavior expectations
Within each domain is a list of strategies to promote improvement. An organizational self-assessment is included at the end to guide leaders through a process to evaluate the gaps within these domains. Prioritize the gaps based found in the first three areas. These are critical for successful culture transformation.
UNDERSTAND THE SAFETY PROFILE OF ADVERSE EVENTS
Examine the patterns to help identify root causes.
Learning from failures is central to building a culture that not only focuses on safety but that makes meaningful improvements for patients, families, and staff in preventing reoccurrences. Examining the contributing factors associated with serious safety events, incident (self-reported safety events) reports and patient complaints can guide leaders in learning where the gaps in culture exist.
Serious safety events or sentinel events are “patient safety events (not primarily related to the natural course of the patient’s illness or underlying condition) that result in death or permanent or temporary harm, or require intervention to sustain life.” (Joint Commission Sentinel Event Policy) Over 80% of the root causes of these events involve ineffective communication, assessment, or leadership. Drilling down to the root causes of each event is time-consuming and requires feedback from all stakeholders, including the patients and families involved. However, collating these results can guide an organization to recognize gaps in the larger culture of safety.
Incident reports about events that cause less harm than serious safety events, or that are near misses, also present an opportunity to identify root causes or contributing factors that highlight enabling factors or enacting behaviors that need to be further assessed and improved. Capturing the root causes of these events is essential in evaluating the cultural factors that need to change.
Patient complaints are often identified through patients’ comments relayed to managers or the patient relations department, either directly or via a satisfaction survey. Recognizing these complaints as safety issues can highlight deficiencies in Safer Culture. Patient reports can identify errors and adverse events that clinicians may have missed or not reported.
ASSESS YOUR SAFER CULTURE USING A VALIDATED INSTRUMENT
Analyze Safer Culture survey data to identify low-scoring domains and worsening trends over time. Then use the Safer Culture framework to identify which enabling factors or enacting behaviors are repeatedly involved as root causes or as low-scoring culture survey domains.
The Joint Commission (11 tenets*) recommends that organizations obtain a baseline assessment of Safer Culture using a validated survey instrument, and repeat the survey every 18–24 months. Several validated surveys are available. Choose one that matches your organizational needs for detecting staff perceptions of specific gaps you may have.
The Agency for Healthcare Research and Quality (AHRQ) established the Surveys on Patient Safer Culture™ and provides step-by-step recommendations for creating an action plan for administering and analyzing patient Safer Culture results. AHRQ also provides a repository for organizations to voluntarily submit their Safer Cultures scores into a national database in order to offer national benchmark data.
INTEGRATE PATIENT/FAMILY INPUT
Include patient and family input in your efforts to understand and improve patient safety across the perinatal continuum. Together, with the other data, the voice of patients and their families can showcase the gaps impeding an effective Safer Culture and direct attention to the factors or behaviors that need further investigation improvement effort.
Carefully analyzing the results of patient satisfaction surveys can disclose helpful information about how your organization communicates and integrates patients and families into the culture of care. AHRQ has many helpful resources to administer and analyze your patient experience surveys.
You can also learn directly from patients and families by enlisting their participation on patient safety initiatives. By sharing patients’ stories and healthcare experiences, healthcare teams and organizational leaders can make improvements that embody the core principles of information sharing, respect, dignity, collaboration and participation inherent in the goal of patient/family centered care.
Developing and empowering patient and family advisory councils to participate with clinicians and leaders on hospital boards, quality councils, and improvement initiatives is also essential. Bringing patients’ stories and experiences to light focuses our attention on the importance to patients, and ultimately helps organizations develop meaningful and sustainable solutions.
The Institute for Patient and Family Centered Care (IPFCC) provides a self-assessment tool* to guide organizations in understanding how they think about and involve patients/families within the hospital culture.
AHRQ offers a step-by-step guide to develop effective patient and family advisory councils within your organization.
*Please contact Maryam Broussard for more information.