Adult Massive Transfusion Protocol
Original Date: 12/2005 | Last Review Date: 10/2025
Purpose: To describe the process of ordering and providing blood and blood components to acutely injured patients.
Overview:
- The goal of the Massive Transfusion Protocol (MTP) is to ensure balanced resuscitation with a transfusion ratio of whole blood or 1:1:1 (plasma: platelets: RBCs) starting with the first units transfused.
- For all patients predicted or suspected of requiring substantial transfusions or in whom the use of uncross-matched blood products is required, MTP should be activated immediately.
- Patients receiving blood products prehospital will automatically have MTP activated.
- Personnel will be sent to retrieve an MTP cooler when a “LEVEL 1 WITH BLOOD” or similar page is sent.
- “LifeFlight to OR” and “Ground EMS to OR” activations will also automatically have MTP activated.
- Blood procurement procedural details are stipulated in the respective activation protocols.
- Patients likely to require MTP are those with two of the following:
- EC arrival heart rate >120
- EC arrival systolic blood pressure < 90 mmHg
- Positive FAST exam
- Penetrating trauma mechanism
- Use of uncross-matched blood in EC
- Positive FAST exam
- Penetrating trauma mechanism
- Use of uncross-matched blood in EC
- Using these parameters, the clinician will be correct 86% of the time (PPV 53%, NPV 96%). This is consistent with the concept of acceptable over-triage and minimizing under-triage.
- Remember: blood products can always be returned and used for another patient but not having the appropriate number/type of products can be a lethal omission.
Massive Transfusion Protocol:
- To activate MTP, the blood bank should be called immediately at 4-3640. Simultaneously, the green blood requisition slip should be “MTP” or “MASSIVE” and sent by a runner to the Blood Bank.
- The requisition slip should NOT include a specific number of products once the MTP is activated.
- The following laboratory tests should be drawn for every Level 1 trauma immediately upon arrival (as soon as clinically possible) and then as clinically indicated:
- Type and Screen, CBC, rapid TEG and ABG/VBG.
- Prioritize the patient’s first blood draw as a Type and Screen for Blood Bank so that universal blood products can be transitioned to type-specific (not fully cross-matched) products as early in the resuscitation as possible. This reduces antibody formation and conserves universal products. This should go to the blood bank immediately after being drawn.
- The initial MTP cooler for all trauma activations (including prehospital activations) will contain six (6) units of low-titer Rh+ group O whole blood. If not enough whole blood supply is available at the time, six (6) packed RBCs, six (6) units of plasma and one (1) dose of platelets will be released instead.
- This initial component-only MTP release will include: six (6) units of O-negative (female)/O-positive (male) RBC and six (6) units of thawed or liquid group A (low anti-B antibody titer) plasma).
- One (1) jumbo plasma may be substituted and is = two (2) to three (3) standard plasma units
- One (1) “dose” of platelets = traditional five (5) pooled random-donor platelet units or one (1) apheresis platelet unit.
- After the first cooler leaves the Blood Bank, a component-only order will be prepared and be available within 5-10 minutes.
- Component order: six (6) RBCs and six (6) plasma and one (1) platelet dose.
- 1 dose of platelets will be issued with every 6 units of RBCs and 6 units of plasma.
- This platelet dose will be repeated after every 6 additional RBCs issued.
- For MTP activations where the patient’s blood type is known, type specific component-only products will be prepared.
- However, if adequate whole blood supplies are available, AND the patient’s blood type is known and is group O, the Blood Bank may release whole blood units instead of component therapy. These coolers may contain 4-6 units of whole blood and no components or separate tackle box of platelets.
- Requests for components exceeding this protocol, as well as cryoprecipitate, may be made at any time by direct notification of Blood Bank (4-3640).
- No blood components will be issued without a pickup slip with the recipient’s medical record number and name.
- Component order: six (6) RBCs and six (6) plasma and one (1) platelet dose.
- Subsequent coolers can be adjusted or modified based on the following rapid TEG values:
-
-
-
ACT > 128 Transfuse plasma and RBC r-value > 1.1 Transfuse plasma and RBC k-time > 2.5 Transfuse plasma
Add cryoprecipitate/fibrinogen if angle also abnormala-angle < 60 Transfuse cryoprecipitate (or fibrinogen)
Add platelets if mA is also abnormalMA < 55 Transfuse platelets
Add cryoprecipitate/fibrinogen if angle also abnormalLY-30 > 3% Administer tranexamic acid or amino-caproic acid
-
- This process will automatically be repeated each time the set of components is issued until the attending Trauma Surgeon, Anesthesiologist, or Circulator Nurse notifies the Blood Bank that the MTP is no longer needed.
-
- Until then, blood coolers should follow the patient at all times to prevent duplicate blood orders and unavailability of blood when needed by the patient.
- When done with the operative case and/or massive transfusion, please contact the Blood Bank to stop the MTP. The phone call can be made by trauma faculty, anesthesia faculty, or a circulator nurse. At this time, unused products should be returned to the Blood Bank unless planned for immediate transfusion.
-
Hemolysis Panel Requirement
- In 2017, MHH-TMC initiated a whole program for use in emergency settings for bleeding patients. The hospital and physician leadership requested we limit the units of whole blood transfused to no more than six (6) units of whole blood based on available data. Based on recommendations from the MHH-TMC Transfusion/Blood Utilization Committee, we began collecting hemolysis panels on all trauma patients emergency release, low-titer, Rh+ group O whole blood (LTO+ WB). This process was discontinued in early 2022 after our research showed no difference between LTO+ WB and component therapy, as well as, no difference between different ABO groups and Rh status patients receiving LTO+ WB.
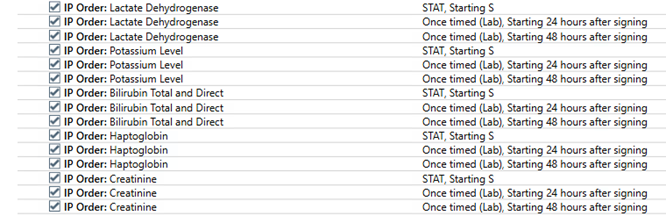
- After approval by all parties and input from the Transfusion/Blood Utilization Committee, the previous “cap”/maximum number of LTO+ WB allowed of six (6) units has been removed. All patients may now receive up to ten (10) units of LTO+ WB, regardless of ABO group or Rh status. Those who are group O may receive greater than ten (10) units based on availability and confirmed type-screen by MHH-TMS Blood Bank. As part of this guideline change, however, we will begin obtaining hemolysis panels at admission, 24 hours, and 48 hours after MTP to closely follow those exceeding six (6) units of LTO+ WB. The hemolysis panel order set has been created in Epic and is named “Whole Blood Hemolysis Evaluation Panel.” In short, LDH, potassium, creatinine, bilirubin, and haptoglobin will be obtained at the three above time points. These orders will be placed by the Trauma Service. Results will be evaluated and presented to the Transfusion/Blood Utilization Committee by Trauma Service representative(s). The order set is shown below.
Whole Blood Hemolysis Panel (ordered on any patient exceeding >6 units of LTO+ WB)