Burn ICU Inhalational Injury Policy
Original Date: 09/2020 | Last Review Date: 12/2024
Purpose: To standardize the work up, classification, and treatment of burn inhalational injuries.
Assessment:
- History and physical to assess risk of inhalational injury
- Mechanism – exposure to smoke, blast injury, steam burns, exposure to caustic fumes
- Intensity and duration of exposure (e.g. patient trapped in enclosed space, found unconscious, etc…)
- Physical Examination:
- Carbonaceous sputum, stridor, hoarseness, drooling, and/or dysphagia are highly suggestive of inhalational injury.
- Facial burns, singed eyebrows or nasal hair, and/or soot deposits on face may also be present, though they alone do not necessarily connote the presence of an inhalational injury.
- Neurologic examination to assess risk of systemic poisoning when appropriate.
- Determine the clinical concern for systemic toxicity:
- Suspected in any patient in an enclosed space fire
- Carbon monoxide poisoning can be difficult to diagnose as they lead to falsely elevated SpO2. A “Blood Gas w/ Coox Panel, Arterial” is necessary for diagnosis
- Alternatively, a venous sample may be obtained using the same order with comments as follows “Please obtain from venous source”
- Cyanide toxicity often occurs with exposure to enclosed space fires involving couches, car seats, cushions, mattresses, etc.
Diagnosis/Management:
- Work up to assess risk of inhalational injury
- Pulse oximetry
- Arterial blood gas with lactate, methemoglobin, and carboxyhemoglobin (COHb) level
- Order “Blood Gas w/ Coox Panel, Arterial”
- Chest x ray
- Determine clinical concern for Carbon Monoxide (CO) Poisoning:
-
- The “COOX” part of the “Arterial Blood Gas w/ COOX” that you ordered – look for COHb
- Remember: SpO2 levels can be falsely elevated in patients with CO exposure, therefore
- While COHb lab is pending, leave patient on 100% FiO2.
- If not intubated, patient should be placed on humidified 100% FiO2 via a non-rebreather until COHb levels return.
- If COHb < 10%, wean FiO2 as tolerated
- If COHb > 10%, continue 100% FiO2 and repeat COHb every hour until the value is <10%.
- The table below depicts the likely symptoms associated with varying levels of COHb
COHb Level Symptoms 0-10 Normal 15-20 Headache, Confusion 20-40 Disorientation, Fatigue, Nausea, Visual Disturbances 40-60 Hallucinations, Combativeness, Coma, Shock 60+ Cardiopulmonary arrest
-
- Determine the clinical concern for Cyanide Poisoning (enclosed fire, unexplained unconsciousness)
- Hydrogen Cyanide is released by combustion of products with synthetic polymers (couches, car seats, cushions, mattresses)
- Cyanide toxicity is difficult to identify in a timely fashion and should be considered empirically in patients who were in an enclosed structure or vehicle fire.
- Administer Hydroxocobalamin (Cyanokit 5g IV) if:
- Lactate levels > 10
- Persistent and unexplained acidosis (unresponsive to IV fluids)
- Unexplained hemodynamic instability (unresponsive to IV fluids)
If given by prehospital personnel, do not give again unless directed by attending.
- The max dose of hydroxocobalamin is 10g (two doses max)
- Hydroxycobalamin can cause transient hypotension, will turn the urine dark red (not rhabdomyolysis), and may stain the skin red.
- NOTE: Hydroxycobalamin has been linked to AKI. It’s use is to be limited to the patient meeting any of the criteria above
- Fiberoptic bronchoscopy is the standard diagnostic test for identifying inhalational injury and should be performed within 2 hours of injury.
Abbreviated Injury Score (AIS) Grade Class Bronchoscopy Description 0 No injury 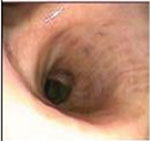
No carbonaceous deposits, erythema, edema, bronchorrhea, or obstruction 1 Mild injury 
Minor or patchy areas of erythema, carbonaceous deposits, bronchorrhea, or bronchial obstruction present 2 Moderate injury 
Moderate erythema, carbonaceous deposits, bronchorrhea, or bronchial obstruction present 3 Sever injury 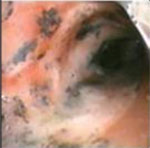
Severe inflammation with friability, copious carbonaceous deposits, bronchorrhea, or bronchial obstruction present 4* Massive injury 
Mucosal sloughing, necrosis, or endoluminal obstruction *There will be patients for whom you have a clinical suspicion for inhalational injury but who do not meet the above criteria. Use discretion when deciding on whether to intubate that patient or consider nasopharyngeal endoscopy.*
- Indications for intubation
- GCS < 8
- COHb level > 20%
- Respiratory failure with hypoxia or hypercarbia
- Extensive face and neck burns (swelling is progressive over the first 48 hours)
- Signs and symptoms of airway obstruction by edema (e.g. hoarseness, stridor, labored breathing, difficulty swallowing)
- Other clinical concern for impending airway obstruction
- Inhalational injury treatments
- All grade injuries:
- Supplemental humidified oxygen
- Nebulized 0.083% albuterol inhalational solution 2.49mg q4 hours inhaled (order under Nebulizer Treatment Orders Adult MPP)
- For Grade 2 and higher injuries, also order:
- Nebulized heparin 10,000 units q4 hours inhaled
- Nebulized 3% sodium chloride 3 mL q4 hours inhaled (order under Nebulizer Treatment Orders Adult MPP)
- High-frequency percussive ventilation (HFPV or VDR) may decrease pneumonia incidence and improve survival. Remains at the discretion of the provider to start it for Grade 3 or 4 Inhalation Injuries.
- When to stop treatment (All grades of injuries):
-
- Extubation
- Resolution of inhalation injury on bronchoscopy
- 7 days of treatment
Inhalation Injury Protocol Grade 0 Grade 1 Grade 2 Grade 3 Grade 4 No treatment Humidified oxygen
Nebulized albuterolHumidified oxygen
Nebulized albuterol
Nebulized heparin q4h
Nebulized 3% NaCl q4hHumidified oxygen
Nebulized albuterol
Nebulized heparin q4h
Nebulized 3% NaCl q4h
Consider HFPVHumidified oxygen
Nebulized albuterol
Nebulized heparin q4h
Nebulized 3% NaCl q4h
Consider HFPV -
- All grade injuries:
- Ventilator management
- Settings:
- No mode of ventilation has been shown to be superior in the setting of inhalational injuries. What HAS been shown to improve outcomes is Lung Protective Ventilatory Strategies (same as ARDS)
- Lung Protective Ventilatory Strategies
- 6-8 mL/kg predicted body weight tidal volumes (Start at 6 mL/kg and can work up to 8 mL/kg if Plateau Pressure allows)
- Plateau pressure < 30 cm H2O
- Driving pressure (Pplat–PEEP) goal <15 cm H2O
- Volumetric Diffusive Respirator (VDR)
- FiO2 95% and titrate to maintain SpO2> 90%. This includes the Fi02 setting on the Vapotherm that is teed in (Vapotherm should be set to 42C and 12-20 lpm of flow).
- Peak inspiratory Pressure (PIP) sufficient to cause apical chest “wiggle” (usually 22 – 32 cmH20).
- Pulse Frequency/Percussive (High Rate) 550 bpm
- Sinusoidal/Convective (Low) Rate 10-12 bpm
- Inspiratory to Expiratory (I:E) ratio – 1:1
- Oscillatory PEEP 7-11 cm H20. Set this value such that it is sufficient to maintain slight chest wiggle.
- Demand PEEP 3 cm H2O (arrow on dial is set at the 3 o’clock position).
- Convective rise is off
- Initial I:E ratio is 1:1. High rate (i:e) ratio is also 1:1 (“arrows up”).
- Endotracheal tube cuff can be partially deflated to assist with CO2 removal
- Airway Pressure Release Ventilation (APRV)
- Pressure high (Phigh) – 2 cm H2O above plateau pressure
- Pressure low (Plow) – 3 cm H2O
- Time high (Thigh)
- Start at 5.2
- Shorten as needed to improve ventilation
- The ideal Thigh is as long a patient can tolerate without inadequate ventilation
- Time low (Tlow)
- Set at 0.8 seconds and watch the volume flow curve
- Decrease Tlow until you cut off the expiratory flow rate at 50-75%
- Settings:
*More information available in the Acute Respiratory Distress Syndrome Algorithm***

Considerations:
- Repeat bronchoscopy:
- For inhalational injuries Grade 2 or higher, consider repeat daily bronchoscopy to assess progression of inhalational injury prior to extubation.
- Utilize the Olympus bronchoscopes for repeat bronchoscopies as they allow improved suction capabilities compared to the disposable bronchoscopes.
- Extubation Criteria:
- Extubate as indicated, including presence of an adequate cuff leak
- Consider the following: Mucosal sloughing and risk of hypoxemia may be delayed up to 72 hours in Grade 2 or higher inhalation injuries
- When to stop Inhalation Injury treatments: (Any of the following criteria are met)
- Extubation
- Bronchoscopy demonstrates complete resolution of inhalation injury
- 7 days of treatment
- If the patient does not tolerate these ventilator strategies, consider:
- Consultation of the ECMO team