Burn VTE Prophylaxis
Burn ICU Venous Thromboembolism Prophylaxis
Original Date: 08/2019
Last Review Date: 12/2024
Purpose: To delineate venous thromboembolism prophylaxis management in the Burn ICU.
If not contraindicated, patients should be treated with BOTH anticoagulation and compression devices.
Mechanical prophylaxis:
- Sequential compression devices (SCD) should be used for all patients.
- SCDs may not be able to be effectively placed on patients with lower extremity burns due to patient discomfort or possible injury to the healing burn wounds and/or skin grafts.
Chemoprophylaxis:
- Low molecular weight heparin (LMWH; enoxaparin) is the VTE chemoprophylaxis of choice and dosing strategy is dependent on patient status upon arrival.
- Floor or IMU patients (non anti-factor Xa dosing):
| Low molecular weight heparin (LMWH) | |
|---|---|
| Patient Weight | Drug Dosing |
| <90 kg | Enoxaparin 30mq q12 hours |
| ≥90 kg | Enoxaparin 40mq q12 hours |
- ICU Patients (anti-factor Xa dosing):
- Calculate the starting enoxaparin dose using the following formula:
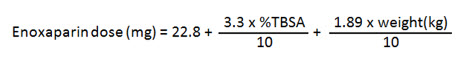
- The calculated dose is rounded to the nearest 10 mg and ordered q 12 hours.
- Calculate the starting enoxaparin dose using the following formula:
- Chemoprophylaxis in patients with kidney failure:
- Unfractionated heparin is used in patients with a CrCl <30mL/min
| Unfractionated heparin (UH) | ||
|---|---|---|
| Patient Weight | Renal Function | Drug Dosing |
| <100 kg | CrCl < 30 ml/min | heparin 5000 units subcutaneous q8h |
| ≥100 kg | heparin 7500 units subcutaneous q8h | |
Anti-factor Xa Dosing:
- Patient Selection:
- Burn ICU patients
- > 20% TBSA burns
- > 15% TBSA full-thickness burns
- < 50 kg or > 90 kg
- Patients with concomitant trauma meeting criteria per trauma division’s guidelines
- For these patients, Anti-factor Xa levels are checked to ensure adequate VTE prophylaxis. The goal Anti-factor Xa level for prophylaxis is 2-0.4. Order a LMWH Anti-factor Xa level 4 hours after the third dose of enoxaparin.
- If the LMWH Anti-factor Xa level is less than 0.2, increase the enoxaparin dose by 10 mg and recheck a LMWH Anti-factor Xa level 4 hours after the third new adjusted dose.
- If the LMWH Anti-factor Xa level is greater than 0.4, decrease the enoxaparin dose by 10 mg and recheck a LMWH Anti-factor Xa level 4 hours after the third new adjusted dose.
- Once the patient has achieved a prophylactic LMWH Anti-factor Xa level, the level should be repeated every 7 days due to the ever changing physiology and volume of distribution.
Holding VTE Chemoprophylaxis
In general, VTE chemoprophylaxis is not held for burn excisions, interventional radiology procedures, or procedures. If a consultant requests the holding of VTE prophylaxis prior to a procedure, please check appropriateness with the appropriate Burn surgeon or intensivist.
Relevant Literature Search:
| Search | Database | Search Term | Limits | Total Yield: # of Articles | # Excluded Articles | # Included Articles |
|---|---|---|---|---|---|---|
| 1 | PubMed | (“deep vein thrombosis” OR “deep venous thrombosis”) AND “burns” | Randomized Controlled Trial, English language, Adults | 7 | 6 | 1 |
| 2 | “ | (“pulmonary embolism” OR “pulmonary emboli”) AND “burns” | Randomized Controlled Trial, English language, Adults | 3 | 2 | 1 |
| 3 | “ | “Xa” AND “burns” | 40 | 33 | 7 | |
| Total | 50 | 41 | 9 | |||
| Excluded: 2 duplicates | ||||||
| Included: 5 papers – 1 RCT (1 duplicate), 2 prospective observational (1 duplicate), 4 Retrospective | ||||||
| Author / Year | Study Type | Patients, n | Inclusion Criteria | Exclusion Criteria | Dosage | Outcomes |
|---|---|---|---|---|---|---|
| McKinzie, 2021 (1) | Retrospective observational | 43 patients | ≥18 years, ≥100 kg or BMI ≥30kg/m2 | Pregnancy, renal failure | 40 mg BID | 42% did not reach therapeutic levels on standard dosing and required dose adjustment |
| Cato, 2021 (2) | Prospective observational | 30 patients | >15% TBSA burns, >18 years | AKI, CKD, other anticoagulant use | Standard enoxaparin dose, followed by increasing doses | 63% had non-therapeutic anti-factor Xa levels on standard dosing |
| Ahuja, 2016 (3) | RCT | 100 (50 enoxaparin, 50 control) | 30-60% TBSA, >18 years | Admitted >2 days after burns, inhalational burns, acute kidney injury, pregnancy | Enoxaparin: 0.5mg/kg twice daily (max 30mg twice daily) | DVT: Enoxaparin: 0/50 (0%) Control: 4/50 (8%) |
| Note: patients received screening ultrasounds to diagnosis DVT, though all patients with a DVT were noted to have clinical symptoms; anti-factor Xa dosing was not available | ||||||
| Constantini, 2013 (4) | Prospective observational | 61 trauma patients | Admission to trauma service and received 3 doses enoxaparin | Started on 30mg BID enoxaparin then anti-Xa levels were checked | -18 (29 -43 (70.5%) were not therapeutic |
|
| Lin, 2011 (5) | Prospective observational | 84 burn patients | >13 years, received 3 doses enoxaparin | Started on weight-based enoxaparin: 30 mg BID standard 5 patients: 40mg BID 2 patients: 50mg BID 3 patients: 60mg BID |
-64 (76%) had sub-therapeutic anti-Xa levels -49 eventually reached therapeutic levels with dose adjustment -15 (18%) were never therapeutic |
|
| Cronin, 2019 (6) | Retrospective | 157 patients | ≥18 years, received 3 doses enoxaparin | Prior DVT, started on non-standard enoxaparin dose | Started on 30mg BID enoxaparin then anti-Xa levels were checked | -81 (51.6%) therapeutic on standard dosing -76 (48.4%) below target anti-Xa level Final dose: 37 (24%) 40mg BID; 10 (6%) 50mg BID, 2 (1%) 60mg BID |
| Faraklas, 2013 | Retrospective | 64 patients | >14 years of age, received enoxaparin, had one or more anti-Xa level drawn | Two groups: -Standard dosing (30 mg BID for BMI 30) -Initial dose calculated using TBSA and weight |
Standard group: 21/31 (68%) subtherapeutic on first anti-Xa level Calculated group: 8/33 (24%) subtherapeutic on first anti-Xa level |
|
References:
- McKinzie BP, Nizamani R, Jones S, King B, Williams FN. Single-center Experience with Venous Thromboembolism Prophylaxis for Obese Burn Patients. J Burn Care Res. 2021;42(3):365-8.
- Cato LD, Bailiff B, Price J, Ermogeneous C, Hazeldine J, Lester W, et al. Heparin resistance in severe thermal injury: A prospective cohort study. Burns Trauma. 2021;9:tkab032.
- Ahuja RB, Bansal P, Pradhan GS, Subberwal M. An analysis of deep vein thrombosis in burn patients (part II): A randomized and controlled study of thromboprophylaxis with low molecular weight heparin. Burns : journal of the International Society for Burn Injuries. 2016;42(8):1693-8.
- Costantini TW, Min E, Box K, Tran V, Winfield RD, Fortlage D, et al. Dose adjusting enoxaparin is necessary to achieve adequate venous thromboembolism prophylaxis in trauma patients. The journal of trauma and acute care surgery. 2013;74(1):128-33; discussion 34-5.
- Lin H, Faraklas I, Saffle J, Cochran A. Enoxaparin dose adjustment is associated with low incidence of venous thromboembolic events in acute burn patients. J Trauma. 2011;71(6):1557-61.
- Cronin BJ, Godat LN, Berndtson AE, Pham A, Kolan S, Box K, et al. Anti-Xa guided enoxaparin dose adjustment improves pharmacologic deep venous thrombosis prophylaxis in burn patients. Burns : journal of the International Society for Burn Injuries. 2019;45(4):818-24.