Controlled Resuscitation in Trauma Patients Clinical Practice Guideline
Original Date: 06/2017 | Last Review Date: 07/2024
Purpose: To standardize blood pressure goals in bleeding trauma patients undergoing active resuscitation.
Recommendations
| Patient population | Recommendation |
|---|---|
| Adult blunt trauma patient without known traumatic brain injury | Resuscitate to a SBP >70 mmHg until hemorrhage is controlled |
| Adult penetrating trauma patient without known traumatic brain injury | Resuscitate to a MAP > 50 mmHg or SBP >70 mmHg until hemorrhage controlled. |
*Note: there is increasing interest in and use of resuscitative balloon occlusion of the aorta (REBOA). When used correctly, REBOA dramatically decreases blood pressure distal to the site of hemorrhage and, as such, is complementary to controlled resuscitation, not contradictory.
Summary of Recommendations/Guideline
For hypotensive patients arriving to the trauma center with penetrating or blunt trauma, resuscitation should be titrated to a systolic blood pressure >70 mmHg until ongoing hemorrhage has been ruled out or control of hemorrhage has been obtained. These patients should receive early blood product utilization and minimal crystalloid administration. Once rTEG data is available it should be used to further guide resuscitation strategies.
Permissive hypotension is not recommended for patients with a suspected traumatic brain injury (maintain SBP>90mmHg) as this could contribute to poor outcomes. Caution should be taken in patients with a preexisting history of hypertension, as their baseline blood pressure may alter the permissive hypotension goal.
Literature Review
Population – adult trauma patients without evidence of traumatic brain injury
Intervention – controlled resuscitation (permissive hypotension) until hemorrhage is controlled
Control – standard of care resuscitation
Outcome – in-hospital mortality
Because of the significance of the mechanism of injury on the possibility of traumatic brain injury, the primary question must be categorized by mechanism and injury pattern:
Primary Question:
Among hypotensive, adult trauma patients, does controlled resuscitation (permissive hypotension) until hemorrhage is stopped decrease in-hospital mortality?
Key Questions to Consider:
- In patients with penetrating trauma, does controlled resuscitation (permissive hypotension) until hemorrhage is stopped decrease in-hospital mortality?]
- In patients with blunt trauma, does controlled resuscitation (permissive hypotension) until hemorrhage is stopped decrease in-hospital mortality?
Methods
To answer these questions, our systematic review must identify evidence that controlled resuscitation (permissive hypotension) either (a) directly reduces mortality or (b) directly reduces the amount of hemorrhage.12 It is reasonable to assume an association between decreased bleeding (theoretical intermediate outcome) and reduced mortality.
Search Strategy
Inclusion criteria:
- Adult trauma patients
- Blunt or penetrating mechanisms of injury
- Outcome = in-hospital mortality
- Randomized controlled trials
- English language
- Human subjects
Databases:
- Pubmed
- Scopus
- Cochrane Database
- Embase
- Published abstracts of the following national trauma associations:
- The American Association for the Surgery of Trauma
- The Eastern Association for the Surgery of Trauma
- The Western Trauma Association
- Podium presentation, quick shots, and posters searched for following terms: hypotensive OR hypotension OR resuscitation.
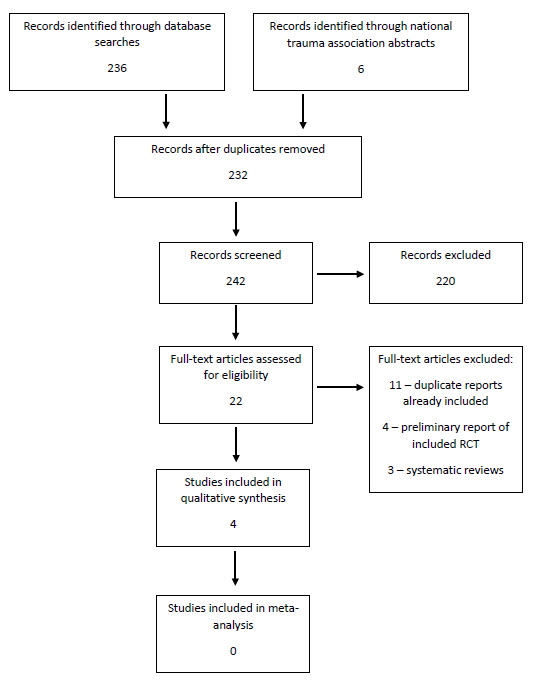
PRISMA Flow Diagram
Grading of Evidence
- In patients with penetrating trauma, does controlled resuscitation (permissive hypotension) until hemorrhage is controlled decrease in-hospital mortality? There is insufficient evidence that controlled resuscitation (permissive hypotension) results in decreased mortality specifically in patients suffering penetrating injuries. The Bickell study showed a dramatic decrease in mortality but was performed in an era where resuscitation was significantly different. Thus, it no longer has external validity. The Carrick study appears to be at significant risk of bias. In it, controlled resuscitation was not found to be superior to standard resuscitation and, given the wide confidence interval, we cannot be sure that it does not increase 30-day mortality. On the other hand, Schreiber’s paper showed a significant reduction in 24-hour mortality for all trauma patients. Given that there are no other studies with a result consistent with Schreiber’s, that there is not necessarily biologic plausibility to the mechanism of injury being a moderator of treatment effect, and that the subgroup was not specified a priori, the reader cannot be sure that the results of the subgroup analysis are not due to chance alone.17 Although the subgroup analysis for penetrating trauma patients failed to show a similar reduction in mortality, those results could be due to chance alone given the methodologic flaws of the subgroup analysis. Thus, we are left with the results of Schreiber’s paper for to state that there is moderate certainty of a substantial benefit to the use-controlled resuscitation in all patients (RRR 65%, NNT 11).Recommendation: Controlled resuscitation (permissive hypotension) should be used in patients with penetrating trauma.
Level of Evidence: Moderate
Net Benefit: Substantial
Grade of Recommendation: B (intervention recommended – there is moderate certainty that the net benefit is substantial) - In patients with blunt trauma, does controlled resuscitation (permissive hypotension) until hemorrhage is controlled decrease in-hospital mortality? In patients specifically with blunt trauma, it is unclear if controlled resuscitation (permissive hypotension) results in decreased mortality. Schreiber’s paper is the only included paper to report the outcomes of blunt trauma patients. The strength of the recommendation is limited by the study design. The mechanism subgroup was not specified a priori. The subgroup analysis for patients suffering blunt trauma is methodologically flawed, as is the subgroup analysis for penetrating trauma patients. Thus, we are left with the results of Schreiber’s paper for to state that there is moderate certainty of a substantial benefit to the use-controlled resuscitation in all patients (RRR 65%, NNT 11).]
Recommendation: Controlled resuscitation (permissive hypotension) should be used in blunt trauma patients without traumatic brain injury.
Level of Evidence: Moderate
Net Benefit: Substantial
Grade of Recommendation: B (intervention recommended – there is moderate certainty that the net benefit is moderate to substantial)
References:
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Injury Prevention and Control [online]. Accessed September 20, 2015.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web–based Injury Statistics Query and Reporting System (WISQARS) [online]. Accessed September 20, 2015.
- Tisherman SA, Schmicker RH, Brasel KJ, Bulger EM, Kerby JD, Minei JP, Powell JL, Reiff DA, Rizoli SB, Schreiber MA. Detailed Description of All Deaths in Both the Shock and Traumatic Brain Injury Hypertonic Saline Trials of the Resuscitation Outcomes Consortium. Ann Surg. Mar 2015;261(3):586-90.
- Davis JS, Satahoo SS, Butler FK, Dermer H, Naranjo D, Julien K, Van Haren RM, Namias N, Blackbourne LH, Schulman CL. An Analysis of Prehospital Deaths: Who Can we Save? J Trauma Acute Care Surg. 77(2):213-18.
- Shackford DR, Mackersie RC, Hoyt DB, Baxt WG, Eastman AB, Hammill FN, Knotts FB, Virgilio RW. Impact of a Trauma System on Outcome of Severely Injured Patients. Arch Surg. May 1987;122(5):523-27.
- Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to Laparotomy for Intra-Abdominal Bleeding from Trauma Does Affect Survival for Delays up to 90 Minutes. J Trauma. March 2002;52(3):420-25.
- Johansson PI, Oliveri RS, Ostrowski SR. Hemostatic Resuscitation with Plasma and Platelets in Trauma. J Emerg Trauma Shock. Apr-Jun 2012;5(2):120-25.
- Kisat M, Morrison JJ, Hashmi ZG, Efron DT, Rasmussen TE, Haider AH. Epidemiology and Outcomes of Non-Compressible Torso Hemorrhage. J Surg Res. 2013;184(1):414-21.
- Shires T, Coln D, Carrico J, Lightfoot S. Fluid Therapy in Hemorrhagic Shock. Arch Surg. Apr 1964;88:688-93.
- Bickell WH, Bruttig SP, Millnamow GA, O’Benar J, Wade CE. The Detrimental Effects of Intravenous Crystalloid after Aortotomy in Swine. Surgery. Sep 1991;110(3):529-36.
- Stern SA, Dronen SC, Birrer P, Wang X. Effect of Blood Pressure on Hemorrhage Volume and Survival in a Near-Fatal Hemorrhage Model Incorporating a Vascular Injury. Ann Emerg Med. Feb 1993;22(2):155-63.