ED Facial Trauma Consult Guidelines
Original Date: 10/2025
The following are a list of facial fractures that DO NOT require an in-person Facial Trauma evaluation. However, please still call Facial Trauma Team to ensure appropriate outpatient follow-up for ALL patients.
This guideline ONLY applies to patients being discharged from the ED.
The EM Team is responsible for performing all physical exam and documentation components.
| Fracture Category | Specific Fracture Pattern | Disposition | Discharge Meds & Instructions | |
|---|---|---|---|---|
| Orbital | 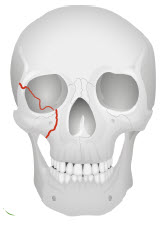 |
Closed, Isolated Orbital Floor or Wall Fracture (diagnosed by CT scan) with exam showing ALL of the following:
If unable to perform eye exam, or have any of the potential injuries above, consult OPHTHO + FACE |
Optho follow up in 48 hours and FACE follow up within 1 week# | Sinus precautions*
If sinuses communicate add antibiotics‡ Nasal decongestant^ |
| Frontal Bone |  |
Closed, isolated anterior table fractures as long as ALL of the following conditions are met:
If the posterior table is involved, must consult NSGY + FACE. |
FACE followup within 1 week# | None |
| Zygomatic Maxillary Complex | 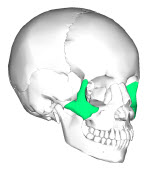 |
Closed, minimally displaced, nondisplaced or isolated temporal arch fracture as long as ALL of the following conditions are met:
|
FACE follow up with in 7-10 days# |
None |
| Nasal | 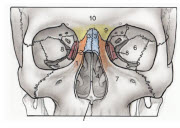 |
Closed, uncomplicated nasal fracture as long as ALL the following conditions are met:
|
FACE follow up within 7 days# | None |
* Sinus precautions for 14 days:
- Avoid forceful blowing of nose
- No smoking or sipping from straws
- Elevated head of bed by 30 degrees
- Always sneeze with mouth open
- Avoid straining with bowel movements
- No flying, swimming, or scuba diving
- No strenuous running or weight lifting
‡Outpatient Antibiotic options:
- Augmentin 875-125 mg PO BID x 10 days
- Keflex 250-500 mg PO QID x 10 days
- Clindamycin 300-450 mg PO TID x 10 days
^Nasal decongestant options (Avoid in patients with uncontrolled hypertension):
- Pseudoephedrine 30mg po Q4-6hrs prn x 3 days max
#Follow up Location/Timing: Please contact on-call Facial trauma resident for specific follow-up attending name and timeframe for all patients
- Plastics: UT Physicians Burn/Plastic Surgery Clinic, 6410 Fannin Street, Suite #1400, Houston, TX 77030, (832)-325-7181
- OMFS: TMC OMFS Clinic, 6411 Fannin Street, Suite Jones Basement #0100, Houston, TX 77030, (713)-704-6500
- ENT: UT Facial Plastic Surgery Clinic, 6400 Fannin Street, Suite #2080, Houston, TX 77030, (713)-486-5019
- Ophthalmology: UT Physician Robert Cizik Eye Clinic Ophthalmology-TMC, 6400 Fannin Street, Suite#1800, Houston, TX 77030,(713)-486-9400
ED Documentation:
- Please utilize the dot phrase “.facialtraumadc” for all patients discharged from the ED without an in-person facial trauma consult.
Appendix for ED Physicians: Eye Injuries Recognition
Ophthalmology should be consulted if there is suspicion of any the following entities as described in the protocol
Optic Nerve Injury
An optic nerve injury, such as optic neuropathy, can occur with a direct blow to the nerve, the bony orbit and canal, or a rapid rise in intra-orbital or intraocular pressure. It can lead to vision loss.
- Clinical Features:
- Sudden, painless loss of vision that may be partial or complete
- Profound decrease in visual acuity.
- Relative afferent pupillary defect (APD) is the most reliable sign and highly concerning
- Ophthalmoscopic exam may appear normal initially, though optic disc pallor (a pale optic nerve head) should develop weeks later.
- Diagnostics:
- Clinical diagnosis based on history and exam, especially the presence of an APD.
- CT scan or MRI of the orbits can help identify the injury, but a normal scan does not rule it out.
Retrobulbar Hematoma
A retrobulbar hematoma is a medical emergency most often due to blunt orbital trauma and characterized by bleeding behind the eyeball, which can lead to increased intraocular pressure and vision loss. It creates an orbital compartment syndrome (OCS) that can cause vision loss within 60-120 minutes.
- Clinical Features
- Eye pain, swelling, a feeling of pressure behind the eye
- Proptosis (exophthalmos): A bulging or forward displacement of the eyeball is highly concerning
- Decreased visual often present
- Elevated IOP > 35 highly concerning
- Afferent pupillary defect (APD) may be present and highly concerning for optic nerve injury
- Diagnostics:
- Clinical diagnosis is often sufficient
- CT scan of the orbits can confirm the presence of a retrobulbar hematoma and show its extent
Traumatic Iritis
Traumatic iritis is inflammation of the iris and ciliary body (the front part of the uvea) due to blunt trauma.
- Clinical Features:
- Gradual onset of pain and light sensitivity within a day or two of the injury, eye pain often not relieved by topical anesthesia
- Blurry vision in affected eye is common
- “Ciliary flush” (Perilimbal conjunctival injection): A ring of redness around the cornea is highly concerning
- Sluggish pupil in affected eye is common
- Often accompanied by a mid-dilated or irregular pupil from iris trauma
- Consensual photophobia (shine light in unaffected eye and patient experiences pain in affected eye) is highly concerning
- “Cells and flare” in the anterior chamber (seen with a slit lamp) is often present
- Diagnostics:
- Slit lamp examination is essential to visualize the anterior chamber if there is concern
Retinal/Vitreous Detachment
A retinal detachment is the separation of the light-sensitive retina from its underlying supportive tissue. A traumatic detachment is a medical emergency that can lead to permanent vision loss.
- Clinical Features:
- New onset of flashing lights (photopsias) or lots of floating spots (floaters) is highly concerning
- Typically painless, except in trauma setting may be associated with pain from trauma (not the detachment itself)
- Visual acuity loss (filmy, cloudy or curtain-like) or visual field loss is highly concerning
- Relative afferent pupillary defect (APD) may be present.
- Slit lamp exam is typically normal.
- Ophthalmologic examination with ophthalmoscope for retinal detachment will reveal a wrinkled, gray retina that is often elevated and mobile and for vitreous detachment will reveal optically empty space with floaters
- Diagnostics:
- Clinical diagnosis is made with a dilated ophthalmoscopic exam, but can be suspected with the above symptoms
- Ocular ultrasound can also be used to visualize the retinal or vitreous detachment
Open Globe Injury
An open globe injury is a full-thickness wound of the eye wall (sclera and/or cornea). It is a surgical emergency that requires immediate consultation.
- Clinical Features
- Eye pain
- +/- Reduced visual acuity may be present
- Irregular or teardrop-shaped pupil highly concerning
- Positive Seidel sign: Leakage of aqueous humor seen with fluorescein staining, appearing as a stream of diluted dye, highly concerning
- Subconjunctival hemorrhage involving entire 360 degree sclera highly concerning
- Scleral or corneal laceration: A visible wound on the surface of the eye is concerning and should raise suspicion
- Diagnostics:
- Clinical suspicion based on exam findings.
- CT scan can show a change in the shape of the globe (e.g., collapsed globe) or a foreign body
Hyphema
A hyphema is the presence of grossly visible blood in the anterior chamber of the eye, as a result of bleeding from the iris/ciliary body
- Clinical Features
- Eye pain is common
- Blurry or decreased vision is common.
- Visible blood in the anterior chamber that layers out forming a “fluid level” which may be subtle or completely fill the space is diagnostic. May be missed if the patient is lying supine on the stretcher. Sit patient upright to appropriately visualize
- Elevated intraocular pressure is a risk, especially with a “total” hyphema (entire chamber filled with blood).
- Diagnostics:
- Clinical diagnosis is made on examination
- Slit lamp examination helps to grade the amount of blood and visualize any associated injuries