Enteral Nutrition Algorithm
Original Date: 08/2011 | Supersedes: 08/2017 | Last Review Date: 09/2021
Purpose: To promote the early use of enteral nutrition and to provide structured multidisciplinary approach so that tolerance can be enhanced and complications can be minimized.
The American Society for Parenteral and Enteral Nutrition publishes and updates guidelines for the assessment and provision of nutrition support in critically ill patients. The recommendations from that guideline were adapted to local culture to create the following Clinical Practice Guideline.
Step One: Nutrition Assessment upon ICU Admission
- Determine if Patient has factors that could contribute to High Nutritional Risk:
- Major trauma
- Severe traumatic brain injuries (GCS<9)
- Abdominal injury requiring laparotomy with bowel resection
- Orthopedic (major pelvic fractures, two or more long bone fractures, amputation)
- Spinal cord injury
- Chronically malnourished patients**
- insufficient PO intake ≤75% for 1 month
- recent weight loss ≥ 5% in 1 month
- muscle and/or subcutaneous fat loss
- Patients with limited physiologic reserve
- Co-morbid disease (lung, liver, kidney disease, active malignancy, immune dysfunction)
- BMI<25 or >35
- Major trauma
- Determine Energy Requirements:
- When available, indirect calorimetry should be used to assess energy requirements.
- In the absence of indirect calorimetry, daily caloric goal should be determined based upon generalized estimates
- BMI : actual body weight x (30 kcal/kg/day)
- BMI >25: ideal body weight +10% x (30 kcal/kg/day)
Step Two: Determine if Patient has a Contra-indication to Enteral Nutrition
- Absolute contraindication to enteral nutrition:
- Bowel obstruction/severe ileus
- Intestinal discontinuity
- Enteral access unattainable
- Relative contraindications to enteral nutrition:
- Blood pressure support with vasopressors
- <0.1 mcg/kg/min norepinephrine (NE)– advance EN slowly and watch for signs of intolerance0.1-0.3 mcg/kg/min NE- consider elemental or peptide-based formula to minimize gut O2 consumption for absorption>0.3-0.5 mcg/kg/min NE – hold EN
- Gastrointestinal bleeding
- Blood pressure support with vasopressors
Step Three: Determine Route of Administration of Enteral Nutrition
- Post-Admission to Feeding Timeline (completed within 4-6 hrs. of ICU admission)
- TF orders: OG or NG tube placement, KUB, tube feeding formula, and pump.
- Clear feeding tube for use
- Tube feeding pump delivered to unit. Tube feeding started at 20mL/hr and advance by 20mL q4H
- Gastric feeds
- Relative contraindications to gastric feeds:
- Respiratory compromise without protected airway (BiPAP, CPAP)
- Foregut surgery (esophagus, gastric reduction)
- Continuous high gastric residual volumes (GRV) *see below
- Unable to elevate head of bed >30◦
- Need for frequent surgery
- Prone position where abdominal exam is difficult
- Relative contraindications to gastric feeds:
- Small bowel feeds
- Patients that should receive small bowel feeding access::
- High risk pts who undergo early laparotomy – place feeding tube at time of initial laparotomy
- Patients undergoing abbreviated laparotomy – place tube at 2nd laparotomy
- All other patients – one attempt at blind placement of “push” NJ made by RN
- Failed “push” NJ attempt—schedule patient for endoscopic placement per ICU team
- Patients that should receive small bowel feeding access::
Step Four: Determine Dose of Enteral Nutrition
-
- Tube feed formulas:
| Patient Condition | Formula | Calories per mL |
|---|---|---|
| Trauma/Critical Care | Peptamen AF® Impact Peptide 1.5 |
1.2 kcal/mL 1.5 kcal/mL |
| Renal failure iHD CRRT |
Novasource® Renal Peptamen AF® |
2 kcal/mL 1.2 kcal/mL |
| Obesity (BMI>35) | Peptamen® Intense (VHP) | 1 kcal/mL |
| Hyperglycemia | Peptamen AF® | 1.2 kcal/mL |
| Diarrhea | Replete® Fiber | 1 kcal/mL |
- Start feeds at 20 mL/hr, advance 20 mL every 4 hours until goal reached
- Standard free water flush is 30mL Q4H
- Gastric feeds: check residuals q4 hours
- If GRV <500mL and:
- No signs of intolerance*, return 300mL aspirate to pt and continue EN, recheck GRV in 4 hrs
- Signs of intolerance* are present, notify MD.
- If GRV ≥500mL and:
- No signs of intolerance*, notify MD, return 300mL aspirate to patient, begin metoclopramide 10mg IV q 6hrs (if metoclopramide already started, add erythromycin IV 250mg q6H), check GRV in 4hrs after metoclopramide dose .
- Signs of intolerance* are present, notify MD.
- If GRV remains ≥500mL after 4 doses of metoclopramide and/or signs of intolerance are present:
- Hold gastric feedings, notify MD, place Small Bowel Feeding Tube, obtain KUB for placement verification, once confirmed initiate EN at 20mL/hr and advance by 20mL/hr q 4hrs to goal rate
- If GRV <500mL and:
*Signs of intolerance: abdominal distention/pain, nausea, emesis, diarrhea, constipation >3 days, a large gastric bubble from x-ray, etc.
Step Five: Additional Nutritional Supplementation
- Trauma
- No high quality evidence to support supplemental micronutrient therapy
Volume-based feeding protocols
- STICU Catch-Up feeding guidelines
-
- If patient receives less than 75% over 5-7 day goal volume due to procedures, a new EN catch-up rate would be calculated.
- The adjusted volume is administered over the following 24-48 hours.
EN catch-up rate = Base rate + base rate × (100% − % of EN volume received)% of EN volume received = EN volume received in the past 24h ×100%24 EN volume goal
- Order catch up rate only if EN reaches goal rate
- Order catch up rate only if EN % < 90% of 24-hour goal volume
- Maximum catch up rate is 150mL/hr
- Do not order catch up rate if any signs of GI intolerance, serum phosphorus < 2.0 or BG >200mg/dL
-
Parenteral Nutrition:
The standard of care in trauma is enteral nutrition. Parental Nutrition should be considered in following situations:
- Supplemental PN in patients not receiving at least 60% of their caloric requirement by day 7-10
- Full PN starting immediately in patients who have no reasonable expectation to reach 60% EN tolerance within the first 7 days of admission (see below)
Contraindications to enteral nutrition:
- Persistent progressive ileus
- Persistent Bowel obstruction
- Significant small bowel resection likely to result in “short bowel syndrome” (~<200cm)
- High-output fistula refractory to enteral nutrition
- Severe Malabsorption
- High risk for nonocclusive bowel necrosis
Criteria for Protein-Calorie Malnutrition:
- Insufficient energy intake
- Weight loss
- Decreased muscle mass
- Decreased subcutaneous fat mass
- Increased fluid accumulation
- Decreased functional status
Moderate or severe protein-calorie malnutrition exists when a patient has ≥2 of the above criteria.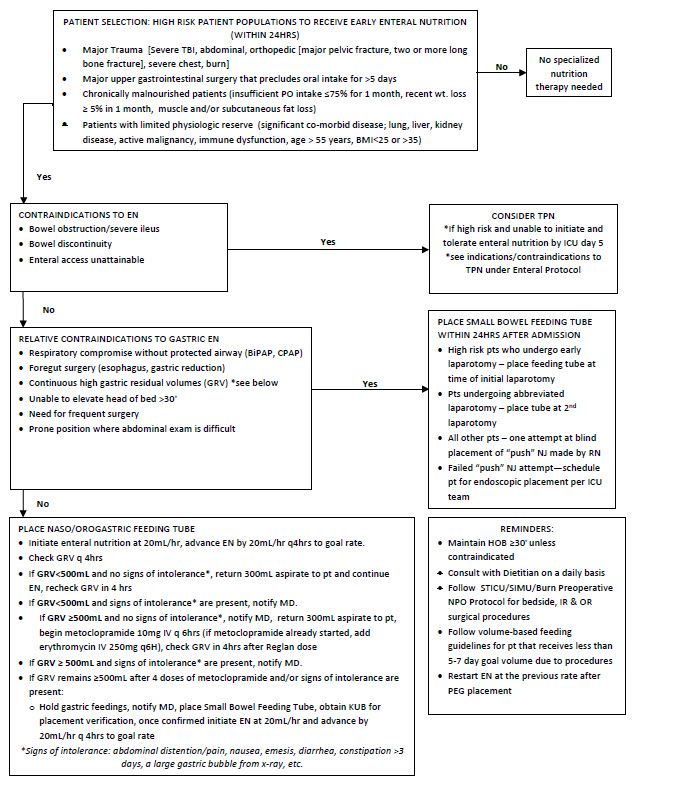
References
- Taylor BE, McClave SA, Martindale RG, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Crit Care Med. Feb 2016;44(2):390-438.
- White JV, Guenter P, Jensen G, et al. Consensus Statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition). JPEN J Parenter Enteral Nutr. 2012; 36:275-283
- Wischmeyer P. Enteral Nutrition Can Be Given to Patients on Vasopressors. SCCM. 2020; 48:123
- Todd SR, Kozar RA, Moore FA. Nutrition support in adult trauma patients. Nutr Clin Pract. 2006 Oct;21(5):421-9. doi: 10.1177/0115426506021005421. PMID: 16998141.
- Braunschweig CL, Levy P, Sheean PM, Wang X. Enteral compared with parenteral nutrition: a meta-analysis. Am J Clin Nutr. 2001 Oct;74(4):534-42. doi: 10.1093/74.4.534. PMID: 11566654.