Evaluation of Genitourinary Trauma
Original Date: 12/2011 | Supersedes: 10/2015, 06/2020 | Last Review Date: 04/2024
Purpose: To guide work up of genitourinary trauma.
The urinary tract may be damaged by a variety of blunt and penetrating mechanisms. The presence of gross hematuria in the trauma patient mandates evaluation for genitourinary injury. This includes evaluation of the kidneys, ureter, bladder, and urethra. The purpose of this policy is to provide guidance for the evaluation of genitourinary trauma. For the purposes of this policy, the following definitions will be used.
- Gross hematuria is defined as blood in the urine that can be seen as a change in the color of the urine.
- Microscopic hematuria is defined as presence of > 3-5 RBC/hpf on microscopy, qualitative analysis on Urinalysis alone is insufficient to diagnose microhematuria. Myoglobin in urine can result in false positive urinalysis
| Grade | Type of Injury | Description of Injury |
|---|---|---|
| 1 | Contusion | Microscopic or gross hematuria, urologic studies normal |
| Hematoma | Subcapsular, non-expanding without parenchymal laceration | |
| 2 | Hematoma | Non-expanding perirenal hematoma confirmed to renal retroperitoneum |
| Laceration | < 1 cm parenchymal depth of renal cortex without urinary extravasation | |
| 3 | Laceration | > 1 cm parenchymal depth of renal cortex without collecting system rupture or urinary extravasation |
| 4 | Laceration | Parenchymal laceration extending through renal cortex, medulla and collecting system |
| Vascular | Main renal artery or vein injury with contained hemorrhage | |
| 5 | Laceration | Completely shattered kidney |
| Vascular | Avulsion of renal hilum which devascularizes kidney |
EVALUATION FOR RENAL INJURY:
- The Gold Standard Assessment of Renal injury includes IV Contrast Enhanced CT Scan including early arterial phase and delayed phase. Optimal timing of delayed urographic phase is 9 min.2
- Absolute indications for renal imaging:
- Gross Hematuria in blunt or penetrating injury
- Microhematuria AND Shock < 90mmHg
- Mechanism of injury- Rapid Deceleration, Injury to Flank, Flank Ecchymosis, penetrating abdominal, flank or lower chest injuries.1
- Significant Renal Injury can occur in the ABSENCE of Gross Hematuria or Microhematuria – if mechanism of injury dictates, pattern of associated injuries or findings on physical exam are concerning- obtain CT as above protocol.
- Microhematuria in isolation is NOT an indication for imaging unless suspicion based on mechanism or physical finding
MANAGEMENT GUIDELINES RENAL INJURY:
- In hemodynamically unstable patients with renal injury with no or only transient response to resuscitation – warrants immediate intervention (Angioembolisation or Surgery)
- Patients who are stable even with high grade injury should be managed non-operatively
- Serial Hgb/Hct and Serial Exams and Close Monitor of vital signs
- Predictors of need for intervention for HG renal injury – Perirenal Hematoma > 4cm, and/or active vascular contrast extravasation in setting of HG renal injury
- Patients with Urinary Extravasation (AAST Grade 4 injury) can be observed initially. 75% of these injuries will heal without intervention
- In patients with medial extravasation of urine without visualization of distal ureter- should increase level of suspicion for UPJ or ureteral injury—should be evaluated and treated early
- Complete UPJ Avulsion Injury Should be managed with definitive repair once patient is stable and should result in prompt urologic consultation
- In unstable patient- Nephrostomy tube to help divert urine
- Any patient with Renal Injury – should be re-imaged in the presence of symptoms of pain, infection, signs of bleeding, or other complications
- Enlarging or infected Urinoma should result in prompt urologic consultation and can be managed with Ureteral Stent, Nephrostomy Tube and/or Urinoma Drain depending on the clinical scenario.
EVALUATION FOR URETERAL INJURIES:
- There are no classic clinical symptoms and signs of ureteral injury, and injury may occur in absence of hematuria. There needs to be a high index of suspicion based on mechanism of injury and location of associated injuries in multi-system trauma, particularly following penetrating abdominal injury, blunt deceleration injuries (particularly in pediatric patients).
- Diagnosis of Ureteral Injury:
- Abdominal and pelvic CT imaging with IV contrast with both immediate early arterial phase and 9 min delayed imaging is the recommended diagnostic study for evaluation of ureteral trauma.2 The following may suggest ureteral injury:
- Asymmetric excretion of contrast
- Contrast Extravasation on delayed imaging
- Medial Contrast Extravasation may suggest Ureteropelvic Junction Injury
- Non-visualization of ureter and extravasation of contrast on delays may indicate injury.
- Single Shot IVP can be performed to assess renal function and evaluate for injury. However, level of detail is minimal
- Direct Inspection in patients suspected of ureteral injury who proceed directly to OR without adequate imaging.
- Can inject 1ampule of Methylene blue IV to aid in diagnosis
- In select situations where evaluation is equivocal, but suspicion is high- retrograde pyelogram may be performed1
- Abdominal and pelvic CT imaging with IV contrast with both immediate early arterial phase and 9 min delayed imaging is the recommended diagnostic study for evaluation of ureteral trauma.2 The following may suggest ureteral injury:
EVALUATION FOR BLADDER INJURIES:
Bladder injuries can be divided into extra peritoneal (60%), and intraperitoneal (30%). Simultaneous extra peritoneal and intraperitoneal injuries occur in 10% of all traumatic bladder injuries.1 About 70–97% of patients with bladder rupture from blunt trauma have associated pelvic fractures. The two most common sign and symptoms are gross hematuria (82%–100%) and abdominal tenderness (62%).1 Other findings may include the inability to void, bruises over the suprapubic region, and abdominal distension. Extravasation of urine may result in swelling in the perineum, scrotum/labia, thighs, and anterior abdominal wall.
- The combination of pelvic fracture and gross hematuria constitutes an absolute indication for immediate cystography in blunt trauma patients.
- Conventional retrograde cystography is the preferred screening method for the evaluation for bladder injury. Bladder should be filled retrograde by pushing contrast with 60cc catheter tip syringe or by gravity. Minimum of 300cc of contrast should be instilled or until patient unable to tolerate. Three views should be obtained. A scout film prior to instillation, at max filling and after complete bladder drainage. Additionally, oblique views can be helpful in particular scenarios, such as evaluating for Bladder Neck Injury.
- Alternatively, CT Cystography can also be utilized, with instillation of a minimum of 300cc of contrast agent into the bladder.
- ANTEGRADE FILLING FROM UROGRAM PHASE AND CLAMPING A FOLEY CATHETER IS NOT APPROPRIATE TECHNIQUE, AND MAY RESULT IN POTENTIAL MISSED INJURY.
- Gross or Microhematuria in patients with penetrating injuries with pelvic trajectory requires cystography, endoscopic (cystoscopy), or direct surgical evaluation of the bladder.
- The presence of isolated microscopic hematuria is not an indication for cystography.
- In patients with microscopic hematuria, cystography imaging should be reserved for those with anterior rami fractures, pubic symphysis diastasis, obturator ring fracture displacement >1cm.5
- Other indicators: inability to void, low urine output, Increased BUN/Cr secondary to peritoneal absorption, abdominal distention, suprapubic pain, and low density free intraperitoneal fluid on CT.
- The presence of pelvic fluid, not otherwise explained by another injury, in patients with pelvic fractures other than acetabular fractures should prompt cystography to evaluate for bladder injury.
EVALUATION FOR URETHRAL TRAUMA
Injuries to the urethra can be partial or complete and complete injury to the posterior urethra related to pelvic fractures are at the junction of the bulbar and membranous urethra. Blood at the meatus is present in 37–93% of patients with urethral injury. Other signs include inability to urinate, perineal/genital ecchymosis (butterfly hematoma of perineum), “high riding” prostate on physical exam. The presence of blood at the meatus should preclude any attempts at urethral instrumentation, until the entire urethra is adequately imaged.
Female Urethral injuries are almost exclusively related to pelvic fracture and more common in children than adults.9 Should be suspected in patients with labial edema and/or blood in vaginal vault on pelvic exam. These should be evaluated by CYSTOCOPY, as RUG is difficult in females, prompt urologic consultation should be initiated.9
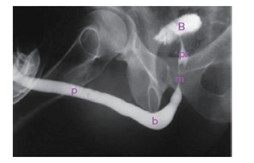
- Retrograde urethrogram (RUG) is considered to be the gold standard diagnostic test for the evaluation of urethral Evaluation for urethral injuries is recommended for the following patients:
- Presence of blood at the urethral meatus
- “High-riding” prostate on rectal examination
- Gross hematuria
- Penetrating trauma to the penis, scrotum, or perineum
- In the event that a Foley catheter has been inserted prior to urethral evaluation (in a patient with concern for urethral trauma) a pericatheter retrograde urethrogram should be performed in a non- emergent fashion to identify a potential missed urethral This is done by injecting contrast via a 5 French ureteral catheter or angiocatheter held in the fossa navicularis to distend the urethra and prevent contrast leak from the meatus.
RETROGRADE URETHROGRAM INSTRUCTIONS:
Where to Perform:
- RUG is optimally performed under fluoroscopy
- In urgent situations, RUG may be performed in the trauma room using digital radiography (DR) equipment
- If possible, depending on injury pattern and if in pelvic binder, patient placed slightly oblique and using a 60cc catheter tip syringe or a 60cc luer lock syringe with a taylor adaptor or 18 gauge angiocatheter and gently inject contrast while keeping the penis on stretch.
- One or more members of the Emergency Radiology team will be present to assist with timing the radiographic exposures and real-time interpretation of the images
Procedure:
- The external meatus is prepared in a standard sterile
- Use either a 60cc catheter tip syringe or a 60cc luer lock syringe with a Taylor adaptor (Pictured on far right) or 18g angiocatheter and insert just into the meatus with lubrication and can push the sides of the meatus against this to prevent contrast from leaking.
- If possible, the patient is rolled in a supine 45° oblique position, with the bottom leg flexed at the knee and the top leg kept straight. The penis should be gently pulled laterally over the proximal thigh using moderate traction on the catheter.
- If patient is stable in a pelvic binder and able to move to fluoroscopy bed, the C-Arm or Fluoroscopy Image Intensifier can be rotated to enable proper orientation and enable you to keep the patient completely supine.
- Gently inject non-dilute Omnipaque-300 and after about 10cc take the first x-ray. Continue to inject contrast slowly and gently, and take another x-ray after another 20cc or so. If there is significant resistance, this may be due to contraction of the external sphincter. Try to have the patient take deep breaths to try to relax the pelvic floor and external sphincter.
- If there is a pelvic fracture related urethra injury you will see extravasation near the level of the inferior pubic ramus and lower aspect of obturator foramen. If there is no visualization of the prostatic urethra or bladder, this is a complete injury. If there is visualization of the bladder with RUG and extravasation, this is an incomplete injury.
- Voiding cystourethrogram, if patient able to void, can provide complete evaluation of the posterior urethra (prostatic and membranous) but largely not applicable in the trauma setting. This requires the same positioning as the RUG and allowing the patient to void while taking x-rays.



EVALUATION FOR GENITAL TRAUMA:
Genital injuries are a result of a wide variety of mechanisms including blunt, penetrating, amputations, bites, burns, or avulsion injuries to the penis, scrotum, testicles in men or vulva in females.
- Scrotal Trauma
- Blunt injury may result in testicular rupture (rupture of the tunica albuginea).
- Scrotal ultrasound should be performed after blunt scrotal trauma or signs/symptoms suggestive of injury.
- Testicular Rupture suspected if U/S demonstrates contour abnormality or heterogeneous echotexture with associated signs/symptoms (testicular pain and scrotal hematoma) and an associated mechanism of injury.
- Prompt surgical exploration and repair or orchiectomy if not salvageable testicle if rupture is diagnoses or suspected.
- Non-operative management of Testicular Rupture is NOT recommended. This can result in testicular atrophy, chronic infection and chronic pain, requiring delayed orchiectomy.
- Scrotal ultrasound should be performed after blunt scrotal trauma or signs/symptoms suggestive of injury.
- Penetrating injury to the scrotum necessitates scrotal exploration, as >50% have testicular injuries. Scrotal ultrasound may not be as reliable in this setting.
- Should have high index of suspicion for associated injuries, including contralateral testicle, spermatic cord structures, corporal bodies, and urethra.
- Blunt injury may result in testicular rupture (rupture of the tunica albuginea).
- Penile Injury
- Penetrating penile injuries should be promptly explored in the stable patient and repair the corporal bodies. The urethra should be evaluated in the same setting and 11-34% of penile injuries have associated urethral injury.11
- Penile Amputation – if the amputated part of the penis is present, this should be wrapped in a saline soaked gauze and put in a plastic bag and then placed on ice in a second bag.
- This should be promptly re-implanted with re-anastomosis of the macroscopic structures and with involvement of plastic surgery for microsurgery for anastomosis of dorsal artery, vein and nerves