Guideline for Cervical Spine Clearance
Original Date: 02/2008 | Supersedes: 12/2011, 06/2014, 10/2014, 06/2017, 09/2021 | Last Review Date: 02/2024 (Reviewed with no changes)
Purpose: To provide a guideline for clearance of the cervical spine. The goal is to facilitate prompt and safe cervical spine clearance for the pediatric trauma patient.
Background
Traumatic spine injuries are reported to occur in 1-3% of pediatric trauma patients presenting for evaluation and treatment to acute care hospitals. It is estimated that 60-80% of these injuries involve the cervical spine. Although, this incidence is low, comparatively speaking, the catastrophic nature of disability which can result necessitates a standardized format for evaluating injuries. Pediatric patients present developmental and anatomic characteristics which make it difficult to assess their risk of cervical spine injury (CSI). Incomplete ossification of the cervical bones, ligamentous laxity and the vertebral configuration of children contribute to the increased propensity of upper cervical spine injuries and ligamentous and neurologic injury without radiographic abnormalities (SCIWORA) in infants and children. In addition, the limited availability of multiple sizes of pediatric extrication collars contributing to poor fit and the prolonged time periods which cervical spine collars are worn prior to clearance contribute to pain, skin breakdown, hygiene issues and other complications for patients. The variability in diagnostic approach and management of c spine injuries has been the impetus for a systematic approach to optimize treatment in pediatric patients with potential or actual cervical spine injuries.
Inclusion
Pediatric trauma patients who present to Children’s Memorial Hermann Hospital with any of the following criteria should be considered for evaluation and treatment with radiographic techniques utilizing this guideline…
- Unconscious patient or patient with abnormal neurologic exam
- Mechanism of injury associated with potential CSI (fall greater than body height, hyperextension injuries, acceleration-deceleration injuries, high speed MVC, bicycle, scooter or ATV accidents)
- Neck pain
- Focal neck tenderness
- Inability to assess neck tenderness due to secondary distracting injury
- Abnormal neurologic examination findings
- History of transient symptomology suggestive of SCIWORA post-trauma (numbness, paresthesias, radiculopathy w/ movement)
- Physical exam findings of neck trauma (ecchymosis, abrasion, deformity, swelling or tenderness)
- Facial or head trauma
- Inconsolable or intoxicated patients who are not reliable for exam
- Unexplained hypotension
Recommendations
- Criteria for clinical clearance of the c-spine for communicative patients ≥ 3 yrs. old:
- Normal mental status
- No alteration in level of alertness
- No age or developmental concerns
- Normal neurologic exam
- Absence of tenderness to cervical spine/soft tissue palpation
- Absence of pain with active range of motion of the neck
- Absence of distracting injuries
- If the patient meets the above criteria, has a negative clinical examination and has a mechanism of injury which is not likely to cause cervical spine injury, radiographic studies of the c-spine may not be indicated. The exam should be documented and cervical collar may be removed.
- Radiographic evaluation of the c-spine: CT Scan of the cervical spine for complete evaluation. Any abnormal radiographic findings or positive exam findings necessitate pediatric neurosurgical consultation.
- Cervical Spine Immobilization: Cervical spine immobilization is indicated for patients who have abnormal radiographs and/or abnormal clinical examination. The absence of radiographic findings solely does NOT ensure it is safe to remove the collar.
- Extrication collars are not designed for prolonged use and oftentimes are not appropriately fit for stabilization of the spine in pediatric patients. A longer-term pediatric cervical collar should be ordered and placed on any patient who is not able have their spine cleared within 2 hrs.
- Recommended Studies: After CT of the cervical spine in patients with positive exams, altered neurologic status precluding examination in trauma patients or positive radiographic findings, MRI of the cervical spine without contrast should be performed in consultation with the pediatric neurosurgeon. If MRI is not available due to metallic restrictions (i.e. ex-fix), implanted devices, recent cardiac surgery or failed sedation, flexion-extension films may be performed for verification of stability of the cervical spine.
- Special Considerations: All pediatric trauma patients who have syndromes and cannot be reliably examined may need pediatric neurosurgery consultations due to the increased risk of pre-existing c-spine instability which may place these patients at risk for further instability post-injury (i.e. Trisomy 18/21, Achondroplasia (Dwarfs), Collagen Vascular Diseases, Ehlers-Danos Syndrome).
Pediatric C-Spine Evaluation Pathway: Reliable1 C-Spine Clinical Exam**
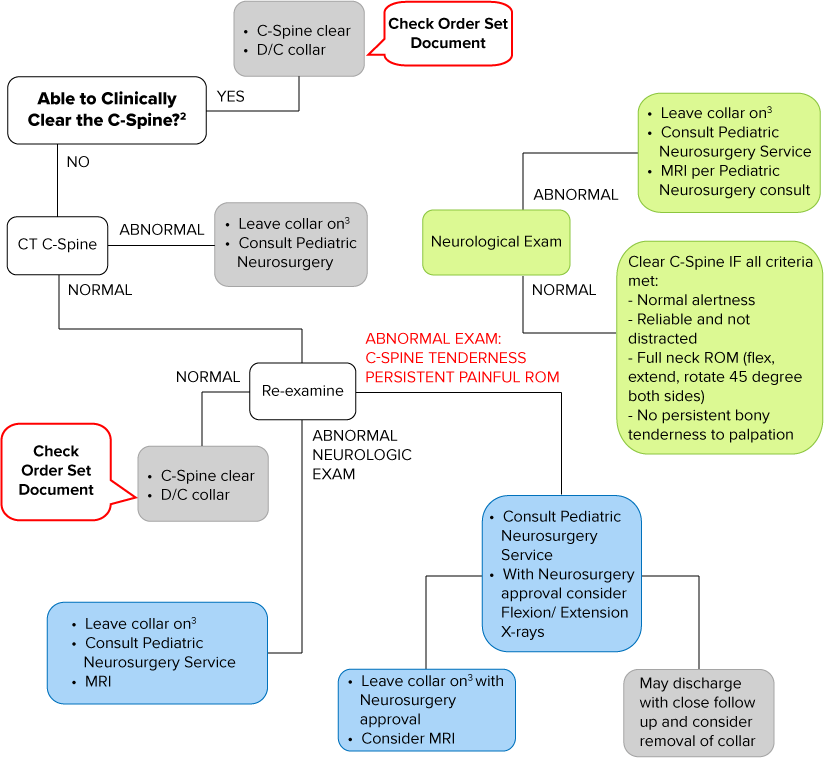
1 Awake and alert with GCS = 15
2 Meet NEXUS criteria AND moves head in flexion/extension AND rotate 45 degrees to both sides with no pain
3 Change to long term cervical spine collar as soon as appropriate
** Adapted from Trauma Association of Canada (TAC) National Pediatric C-Spine Evaluation Pathway: Reliable1 Clinical Exam (April 2011)
Pediatric C-Spine Evaluation Pathway: Unreliable1 Clinical Exam**
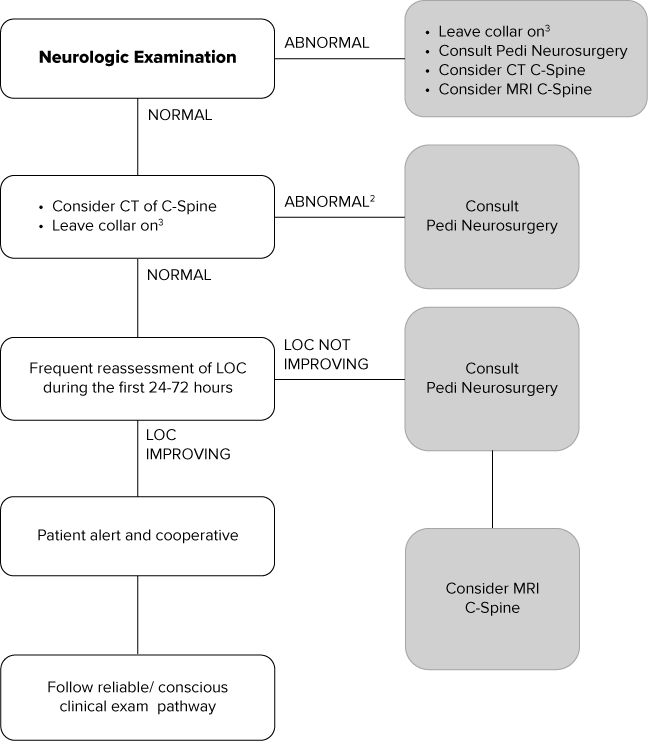
1 Unconscious or decreased level of consciousness with GCS < 15
2 Consider T/L spine injury in those with a documented C-spine injury
3 Change to long term cervical spine collar as soon as appropriate
** Adapted from Trauma Association of Canada (TAC) National Pediatric C-Spine Evaluation Pathway: Unreliable1 Clinical Exam (April 2011)
References
Trauma Association of Canada Pediatric Subcommittee National Pediatric Cervical Spine Evaluation Pathway: Consensus Guidelines. Journal of Trauma, 2011;70: 873-884
Trauma Association of Canada Pediatric Subcommittee National Pediatric Cervical Spine Evaluation Pathway: Consensus Guidelines. Journal of Trauma, 2011;70: 873-884
Anderson, R., Kan, P., Hansen, K., & Brockmeyer, D. (2006). Cervical spine clearance after trauma in children. Neurosurgery Focus, 20(2), E3
Cirak, B., Ziegfeld, S., Knight, V., Chang, D., Avellino, A, & Paidas, C. (2004). Spinal injuries in children. Journal of Pediatric Surgery, 39(4), 607-612
Insko, E., Gracias, V., Gupta, R., Goettler, C., Gaieski, D., & Dalinka, M. (2002). Utility of flexion and extension radiographs of the cervical spine in the acute evaluation of blunt trauma. Journal of Trauma Injury, Infection and Critical Care, 53(3), 426-429
Kokoska, E., Keller, M., Ratio, M., & Weber, T. (2001). Characteristics of pediatric cervical spine injuries. Journal of Pediatric Surgery, 36(1), 100-105
Lee, S., Sena, M., Greenholz, S., & Fledderman, M. (2003). A Multidisciplinary approach to the development of a cervical spine clearance protocol: Process, rationale, and initial results. Journal of Pediatric Surgery, 38(3), 358-362
Meyet, P., Trabold, F., Orliaguet, G., Blanot, S., Renier, D., & Carli, P. (2005). Combined high cervical spine and brain stem injuries: a complex and devastating injury in children. Journal of Pediatric Surgery, 40, 1637-1642
Neurosurgery: Guidelines for the Management of Pediatric Cervical Spine and Spinal Cord Injuries. (2002). Neurosurgery, 50(3 Suppl.), S85-S99