Initial Management of Blunt Thoracic Aortic Injury
Original Date: 03/2015 | Last Review Date: 06/2023
Purpose: To delineate the initial management of blunt thoracic aortic injuries.
Summary Statement:
Blunt thoracic aortic injury (BTAI) is potentially lethal and often associated with severe multi-system injury. BTAI has a broad range of severity and acuity of presentation. Initial workup should be focused upon accurate anatomic identification and categorization of the aortic injury and assessment of associated injuries. This information will be evaluated jointly by the trauma team and the vascular team to establish treatment priorities and formulate therapeutic plans as outlined below.
Diagnosis:
- Patients with severe blunt chest trauma, especially those with deceleration-type injuries, will be evaluated using CT of the chest with IV contrast per current trauma service protocol.
- CT should be used liberally in patients with significant mechanism of injury.
Grading of Injuries:
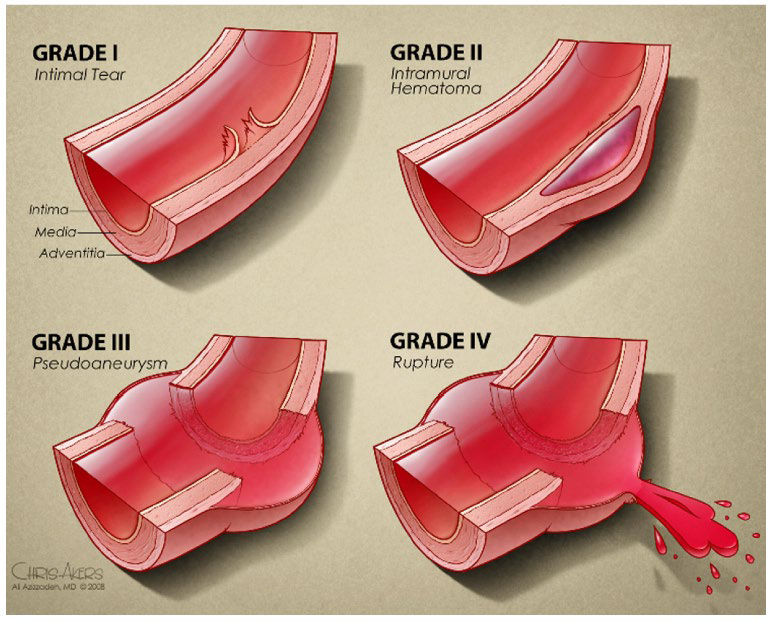
- Injuries will be graded according to the current Society of Vascular Surgery (SVS) guidelines.(1) (See notes section for graphical representation)
- Grade 1 – Intimal tear (normal external contour of aorta)
- Grade 2 – Intra-mural hematoma
- Grade 3 – Pseudoaneurysm
- Grade 4 – Pseudoaneurysm with rupture
Initial Medical Management:
- All patients with aortic injuries should have active control of blood pressure and heart rate with β blockade to minimize wall shear stress and decrease potential for expansion or rupture.
- Therapeutic targets are: SBP < 120, MAP < 80, and pulse < 90.
- If SBP >120 or pulse > 90, start Esmolol 500 μg/kg slow bolus over 30 seconds, if BP remains > 120 repeat 500 μg/kg slow bolus over 30 seconds. Use caution, titrate carefully to avoid hypotension (SBP < 80 or MAP < 60)
- Start infusion at 50 μg/kg/min
- Titrate drip to achieve target SBP, be cautious to avoid hypotension (SBP<80, MAP< 60) especially in patients with potential brain injury
- Stable patients without need for ICU admission may receive oral beta-blocker
Treatment:
- Grade 1 injuries are generally managed medically with repeat imaging as indicated.(2-7)
- Grade 2 injuries may be managed medically or by TEVAR. Therapeutic plans should be made jointly.(3-5, 7, 8)
- Grade 3 injuries without high-risk features should undergo TEVAR within 24 hours after admission.(3, 4, 7)
- Specific therapeutic plans, including order and timing of interventions, should be established jointly after consideration of all associated injuries, most importantly the presence of severe brain injury
- Grade 3 injuries with high-risk features should undergo emergency TEVAR.(1,3-5)
- High risk features include:
- Aortic arch hematoma
- Ascending aortic, aortic arch, or great vessel involvement
- Mediastinal hematoma causing mass effect
- Posterior mediastinal hematoma > 10 mm
- Lesion to normal aortic diameter ratio > 1.4
- Pseudocoarctation of the aorta
- Large left hemothorax
- High risk features include:
- Grade 4 injuries should undergo emergency TEVAR. These patients have substantial risk of decompensation and death.(3-5)
Medical Management:
- Anti-platelet therapy:
- Given for all grade injuries and for medically and surgically treated patients as allowed by concomitant injuries.
- Dose: 81 mg per day.
- For patients treated with TEVAR they will take 81 mg for 30 days post-op
- For patients treated medically they will take 81 mg until injury resolves on imaging
- Blood pressure and heart rate targets:
- Non-operative management: transition esmolol drip to oral beta blockers to goal SBP<120 mmHg and pulse <90.
- After repair: no blood pressure management required after endovascular coverage of the injury
- For patients treated medically, impulse control goals with oral beta blockers will continue until injury resolution seen on imaging
Follow up:
- Repeat imaging is not needed inpatient after TEVAR
- Repeat imaging inpatient for patients treated medically will be done on select patients as decided by the vascular team
- All patients with BTAI should have follow-up CTA scheduled at about 6 weeks post injury
- All patients with BTAI should have appropriate follow-up with vascular surgery.
Notes:
- Grade 3 encompasses a heterogenous group including both small, stable pseudoaneurysms as well as larger unstable ones. Additional characteristics of the injury pattern and imaging may help to predict increased likelihood of rupture, including the size of the pseudoaneurysm, the extent of mediastinal hematoma, especially in the dependent portion of the mediastinum, and the presence of unexplained left hemothorax.
Search Strategy
| Search | Database | Search Term | Limits | Total Yield: # of Articles | # Excluded Articles | # Included Articles |
|---|---|---|---|---|---|---|
| 1 | PubMed | “blunt aortic injury” OR “blunt traumatic aortic injury” | Randomized controlled trial | 0 | 0 | 0 |
| 2 | PubMed | “blunt aortic injury” OR “blunt traumatic aortic injury” | Systematic review | 3 | 1 | 2 |
| 3 | PubMed | “blunt aortic injury” OR “blunt traumatic aortic injury” | None | 170 | 160 | 10 |
| Total | 172 | 161 | 11 | |||
| Exclude Multiples 1 | ||||||
| Included Papers 10 (0 RCTs, 0 Observational, 1 SR/CPG, 8 Retrospective, 1 Expert Opinion) +2 Non identified in search (1 SR/CPG, 1 Retrospective) |
||||||
Literature Review
| Author/Year | Study Type | Inclusion | Conclusions | Comments |
|---|---|---|---|---|
| Isselbacher, 2022 | Clinical Practice Guideline | – Updated high risk features for Grade 3 injury | ||
| Gaffey, 2019 | Retrospective cohort | Grade II BTAI | Grade II injuries may be safely managed non-operatively | 15 patients |
| Quiroga, 2019 | Retrospective cohort | BTAI | Minimal injuries may be managed medically. Moderate injuries can be repair semi-electively. | 87 patients |
| Spencer, 2018 | Retrospective cohort | Grade II BTAI | Grade II injuries may be safely managed non-operatively | 8 patients |
| Heneghan, 2016 | Retrospective cohort | BTAI | -Minimal injuries: no external contour abnormality; intimal tear or thrombus 1 cm; treatment semi-elective -Severe injuries: active extravasation; left subclavian artery hematoma >1.5 cm; emergent repair |
|
| Harris, 2015 | Retrospective cohort | High grade BTAI | High risk if any of the 2 are present: -Lactate >4 mMol/L -Mediastinal hematoma >1 cm -Lesion/normal aortic ratio >1.4 |
|
| Fox, 2015 | Clinical Practice Guideline | -CT appropriate imagining for diagnosis -Endovascular repair preferred over open -Effective blood pressure management during delay to repair |
||
| Osgood, 2014 | Retrospective cohort | Grade 1 and 2 BTAI | Progression of Grade 1 and 2 injuries is rare (5%) | 49 patients |
| Lamarche, 2012 | Expert opinion | BTAI | Different grading system | 48 patients |
| Starnes, 2012 | Retrospective cohort | BTAI | No patient with a normal external contour of the aorta died. Patients with intimal tears can be treated non-operatively. If a pseudoaneurysm it to rupture, it will do so early. |
140 patients |
| Lee, 2011 | Clinical Practice Guideline | Overall weak recommendations: -Endovascular repair preferred over open -Suggests repair within 24 hours |
||
| -Non-operative management of Grade I injuries -Selective left subclavian revascularization -Low dose systemic heparinization |
||||
| Paul, 2011 | Retrospective cohort | Minimal BTAI | Patients with minimal BTAI should be managed non-operatively | 15 patients |
| Azizzadeh, 2009 | Retrospective cohort | BTAI | Grade 1 – intimal tear Grade 2 – intimal hematoma Grade 3 – pseudoaneurysm Grade 4 – rupture |
71 patients |
References
4. Harris DG, Rabin J, Kufera JA, et al. A new aortic injury score predicts early rupture more accurately than clinical assessment. Journal of vascular surgery 2015;61:332-8.
- Azizzadeh A, Keyhani K, Miller CC, 3rd, Coogan SM, Safi HJ, Estrera AL. Blunt traumatic aortic injury: initial experience with endovascular repair. Journal of vascular surgery. 2009;49(6):1403-8.
- Paul JS, Neideen T, Tutton S, Milia D, Tolat P, Foley D, et al. Minimal aortic injury after blunt trauma: selective nonoperative management is safe. J Trauma. 2011;71(6):1519-23.
- Lee WA, Matsumura JS, Mitchell RS, Farber MA, Greenberg RK, Azizzadeh A, et al. Endovascular repair of traumatic thoracic aortic injury: clinical practice guidelines of the Society for Vascular Surgery. Journal of vascular surgery. 2011;53(1):187-92.
- Heneghan RE, Aarabi S, Quiroga E, Gunn ML, Singh N, Starnes BW. Call for a new classification system and treatment strategy in blunt aortic injury. Journal of vascular surgery. 2016;64(1):171-6.
- Starnes BW, Lundgren RS, Gunn M, Quade S, Hatsukami TS, Tran NT, et al. A new classification scheme for treating blunt aortic injury. Journal of vascular surgery. 2012;55(1):47-54.
- Osgood MJ, Heck JM, Rellinger EJ, Doran SL, Garrard CL, 3rd, Guzman RJ, et al. Natural history of grade I-II blunt traumatic aortic injury. Journal of vascular surgery. 2014;59(2):334-41.
- Quiroga E, Starnes BW, Tran NT, Singh N. Implementation and results of a practical grading system for blunt thoracic aortic injury. Journal of vascular surgery. 2019;70(4):1082-8.
- Gaffey AC, Zhang J, Saka E, Quatromoni JG, Glaser J, Kim P, et al. Natural history of non-operative management of Grade II blunt thoracic aortic injury. Annals of vascular surgery. 2019.