Pediatric Massive Transfusion Protocol (P-MTP)/ Emergency Release of Blood from Blood Bank
Supersedes: 08/2011, 05/2012, 08/2013, 06/2017, 09/2021 | Last Review Date: 08/2023
Purpose: To describe the process of rapidly providing the appropriate number and composition of blood and blood components to the acutely injured pediatric patient.
Procedure
Initial Transfusion:
- Notify Blood Bank (4-3640) immediately of an urgent need for blood. At a minimum, inform the Blood Bank how many RBCs are needed and how they should be issued:
- O Negative Uncrossmatched (available immediately; ready within 10 minutes from notification)
- Type-Specific Uncrossmatched (available 15-20 min; requires a specimen)
- Completely Crossmatched (available 60 min; requires a specimen)This will ensure that a cooler is ready for pickup when a runner arrives. If possible, let the Blood Bank know the type of trauma as well. A blood sample (labeled with a red armband label and patient’s first name, last name, and MR number) must be sent to the Blood Bank for a Type & Cross. The collector’s initials, date, and time of collection must be on the sample label. The Emergency Release of Blood form must be completed with the patient’s name and number, the estimated age and weight, the estimated total blood volume, the number of RBCs and FFP needed, and signature of the requesting physician/designee. This form must be taken by a designated runner to the Blood Bank. Units will not be issued without a medical record number.
- If the blood type is unknown and the team cannot wait for type-specific RBCs, O Negative RBCs will be issued.
- If O Neg RBCs have been issued and a sample is still unavailable for typing, the patient may be switched to O Pos RBCs.
- All RBCs will be transfused in the standard manner. All patients must be identified (name and MR number) prior to transfusion.
- The Pediatric Massive Transfusion Protocol (P-MTP) should be initiated as soon as the Pediatric Surgery, Trauma or Anesthesiology attending recognizes that a patient will require massive transfusion (see Indications, under #8). The MTP must be initiated with a telephone call to the Blood Bank (4-3640) by a nurse or healthcare provider from the requesting location, stating massive transfusion, the physician name, the patient name and MR#. The pedi massive procedure is activated by a physician.
- Pediatric Massive Transfusion Protocol:
- Within 10 minutes of notification of a P-MTP, the Blood Bank will have one set of RBCs, Plasma (number of units depend on child’s estimated weight; see Table 1) packed in a cooler, and Platelets (see table 2) available for runner pickup. If Plasma is not immediately available (based on type of patient), the Blood Bank will issue units that are ready and notify appropriate personnel when the remainder is thawed.
- The second set of RBCs, Plasma and platelets will be issued and will be repeated as long as needed. The result of the TEG should be taken into consideration. If non ABO compatible platelets will be provided, the blood bank will notify the attending by phone.
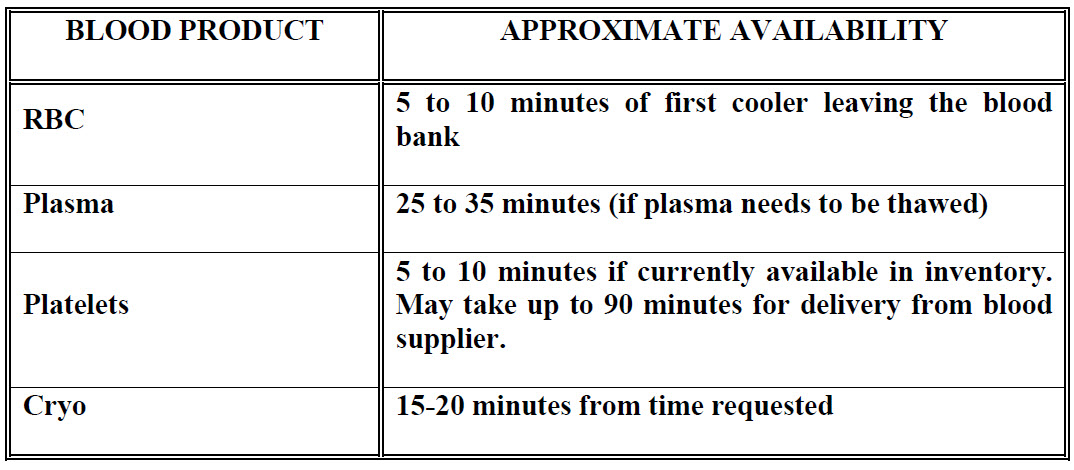
- After the first cooler leaves the Blood Bank (#1 above), the Blood Bank will then prepare the next set of RBCs, Plasma (or 1-2 Jumbo Plasma), and Platelets. This component order will be available based on the chart below. This process will automatically be repeated each time the set of components is issued until the attending Pediatric Surgeon, Trauma Surgeon, Anesthesiologist, or Pediatric Intensivist notifies the Blood Bank that the P-MTP is no longer needed.
- Blood coolers should follow the patient at all times to prevent duplicate blood orders and unavailability of blood products when needed by the patient.
- No blood component will be issued without a pickup slip with the recipient’s medical record number and name.
- Laboratory tests should be drawn initially and then as clinically indicated (at least after each cooler of products has been transfused).
- CBC, PT, aPTT, Fibrinogen
- TEG, if available
- Indications for Pediatric MTP include, but are not limited to:
- Massive bleeding/trauma patient
- Massive blood loss with profound hemorrhagic hypovolemic shock
- >50% of total blood volume loss in 3 hours with continuous bleeding
- When you are done with the operative case and/or massive transfusion, please contact Blood Bank and stop the MTP. The phone call can be made by the Trauma Faculty, Anesthesia Faculty, Circulator Nurse, emergency center nurse or PICU nurse.
- Ice Block Monitoring/Replacement:
- The ice blocks must be replaced in the blood cooler every 6 hours. Blood Bank personnel will monitor this process and notify the nursing unit when the blood cooler needs to have the ice blocks replaced.
- Personnel from the nursing units will pick up new ice blocks from the Blood Bank and transport them to the patient’s location in an ice-block transport cooler.
- Nursing personnel will place the new ice blocks in the blood cooler after removing the current ice blocks.
- The ice blocks removed from the blood cooler should be placed in the ice-block transport cooler and returned to the Blood Bank.
- Nursing personnel will remove the date and time tape from the ice-block cooler and place it on the blood cooler when the ice blocks are replaced.
- Nursing personnel will place the new ice blocks in the blood cooler after removing the current ice blocks.
- Nursing personnel should check blood component expiration dates when the ice blocks are replaced to ensure nothing in the blood cooler is close to expiring.
- Ice blocks will NOT be placed in any cooler or refrigerator that is not maintained by Blood Bank.
- If the blood components in the bedside cooler have not been utilized after six (6) hours, or if the patient’s condition stabilizes, return the blood cooler and blood components to the Blood Bank instead of replacing the ice blocks
For TEG guidance please refer to https://med.uth.edu/surgery/rteg-based-goal-directed-hemostatic-resuscitation-in-high-risk-pediatric-trauma/
Reference:
ACS TQIP Massive Transfusion in Trauma Guidelines
Table 1
Numbers of RBC’s, FFP and Platelets to be prepared according to patient’s weight
| 0-10 kg TBV < 800ml | 3 units PRBC | 3 units FFP | ½ apheresis unit Platelet |
| 11-20 kg TBV 900 -1800ml | 4 units PRBC | 4 units FFP | 1 apheresis unit Platelet |
| 21-40 kg TBV 1800 -3200ml | 5 units PRBC | 5 units FFP | 1 apheresis unit Platelet |
| > 40 kg TBV > 3200ml | 6 units PRBC | 6 units FFP | 1 apheresis unit Platelet |
Table 2
| Pediatric Trauma Massive Transfusion Guidelines | |
|---|---|
| FFP/FP24 | As soon as the need for massive transfusion is recognized, no later than after 50% of patient’s blood volume has been replaced. For every RBCs, give FFP/FP24 (1:1 ratio) NOTE: 1 Jumbo FFP/FP24 = 2 FFP/FP24 |
| Platelets | After 3 units each RBC and FFP, give 1/2 dose platelets. |
| Cryoprecipitate | Fibrinogen based: After one total blood volume has been replaced, check fibrinogen level. If <200 mg/dL, give 1-2 units/10 Kg of cryoprecipitate. Repeat as needed, depending on fibrinogen level, and request appropriate amount of cryo.
TEG based: If α < 60 on TEG give 10 ml/kg cryoprecipitate. NOTE: FFP/FP24 also contains fibrinogen and thus cryoprecipitate is not frequently needed. |
Table 3
| PATIENT’S WEIGHT (Kg) | NUMBER OF RED CELL UNITS TO EQUAL TOTAL BLOOD VOLUME |
|---|---|
| <11.5 | 2 |
| 11.6 – 17.5 | 3 |
| 17.6 – 26.5 | 4 |
| 26.6 – 33.0 | 5 |
| 33.1 – 40.0 | 6 |
| 40.1 – 46.5 | 7 |
| 46.6 – 53.0 | 8 |
| 53.1 – 60.0 | 9 |
| > 60.0 | 10 |