Management of Hemodynamically Significant Pelvic Fractures
Original Date: 12/2013 | Supersedes: 11/2019, 06/2020 | Last Review Date: 04/2024
Purpose: To develop a protocol to ensure rapid identification and treatment of hemodynamically significant pelvic fractures.
Background: Patients in hemorrhagic shock due to pelvic fractures present complex clinical problems.
Common errors in the treatment of these patients include:
- Failure to apply a pelvic binder to an open book pelvis
- Failure to identify and correct coagulopathy
- Misidentification of source of hemorrhage (or missing additional / contributing sources of hemorrhage – most commonly in blunt polytrauma patients)
- Failure to rapidly triage patient to the hybrid operating room
- Patients stay in the Emergency Department too long
- Failure to rule out concomitant perineal, urologic or rectal injury
Indications for AP Pelvis Films during Trauma Resuscitation:
- Hemodynamic instability
- Pelvic pain or tenderness
- Instability of pelvis on physical exam
- Suspicion of femur fractures
- Suspicion of hip dislocation
- Perineal trauma
- Intubated patients (s/p high mechanism trauma)
Applying a Pelvic Binder:
- Indications:
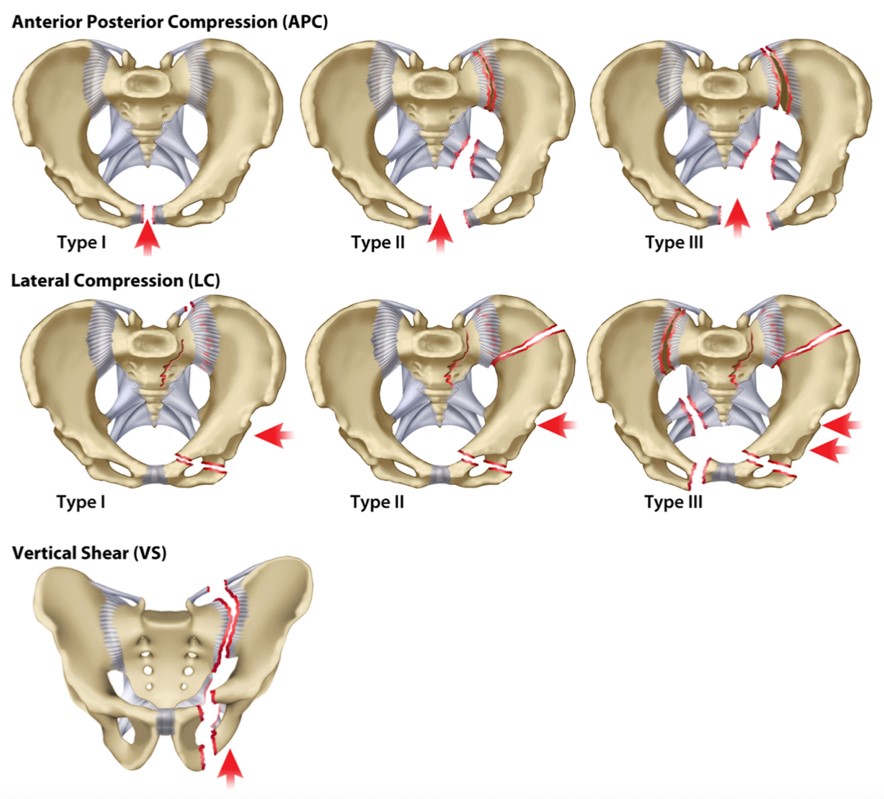
- Any open book pelvic fracture (APC-I, APC-II, APC-III)1 despite hemodynamic status
- A patient with a suspected pelvic fracture and hemodynamic instability, where pelvic films are not available.
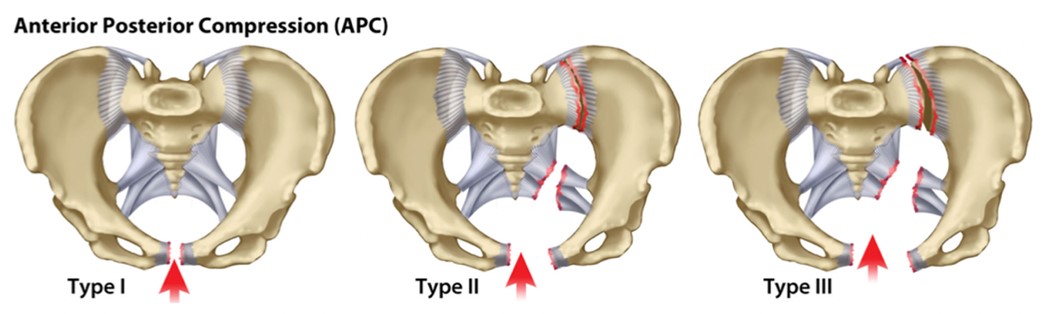
Alton & Gee, 2014.
- Steps:
- Pelvic binder should be centered over greater trochanters.
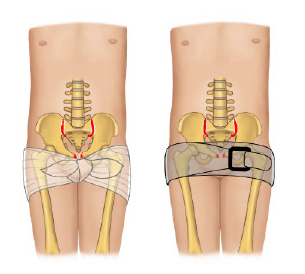
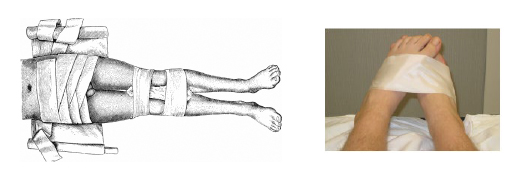
- If access to groins is necessary, move binder to mid-thigh or knees and tape feet together.
- Before leaving trauma bay, ensure thorough evaluation for perineal/rectal/urologic injury
- If concern for urethra / bladder injury is present, Retrograde Urethrogram (RUG) & Cystogram should be completed after CTA abdomen/pelvis with IV contrast 3,5
- Pelvic binder should be centered over greater trochanters.
Contraindications to pelvic binder: None*
- Lateral compression fracture patterns (LC I, II, III) can be worsened by inappropriate application of pelvic binder.
Identification and Treatment of Coagulopathy:
- Obtain intravenous access above the diaphragm (upper extremity, chest, or neck)
- Controlled resuscitation, permissive hypotension: don’t “pop the clot”
- Systolic blood pressure goal >70 mmHg
- MAP > 50 mmHg
- Hemostatic resuscitation:
- Minimize crystalloid and colloid administration
- Resuscitate with 1:1:1 ratio of RBCs:FFP:platelets
- Give FFP and platelets early
- Rapidly identify source of bleeding and definitively control hemorrhage.
- Early placement of ultrasound-guided Common Femoral arterial line, to facilitate possible REBOA placement in hemodynamically unstable pelvic fractures
- Correct TEG and reverse anti-coagulant/anti-platelet medications as indicated
Identify Source of Bleeding:
- Chest radiograph to evaluate for hemothorax/tension pneumothorax
- Pelvic radiograph to evaluate for and identify type of pelvic fracture.
- Place pelvic binder if patient is found to have an open book pelvis (APC I, II, III)
- Contact orthopedic surgery resident immediately (4-BONE)
- FAST exam:
- FAST Negative and non-responder:
- Consider diagnostic peritoneal aspiration (DPA) to rule out concurrent intra-abdominal hemorrhage
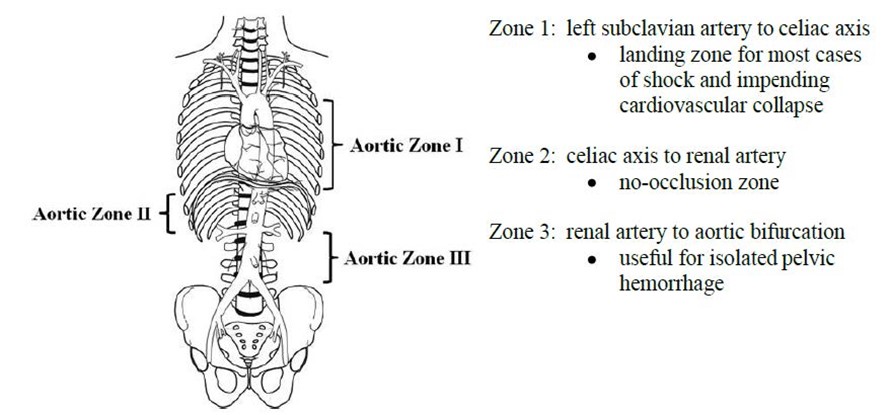
- Consider Zone III REBOA placement prior to transport
- Adequate placement at aortic bifurcation can be ensured by the loss of the contralateral femoral pulse.
- Proceed to angiography / hybrid operating room +/- pre-peritoneal packing
- FAST Positive and patient non-responder
- Consider zone I REBOA placement prior to transport
- Proceed to hybrid OR for laparotomy +/- angiography +/- pre-peritoneal packing
- FAST Negative and non-responder:
- If patient has a sustained response to initial resuscitation:
- Proceed to CT for further imaging, or to operating room if indicated by clinical picture (traumatic diaphragm injury, intra-abdominal bleeding, evisceration).
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA)
Once in the hybrid operating room, the two most common therapeutic interventions are:
- Pre-peritoneal pelvic packing (PPP)4,6
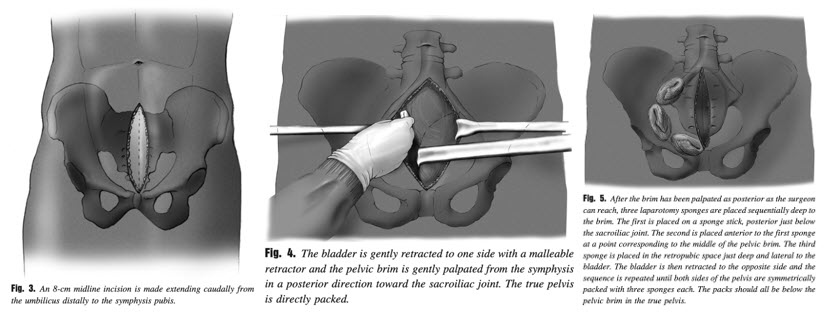
- Infraumbilical vertical midline incision (~8cm) to just above pubic tubercle.
- In a large pelvic hematoma, the pre-peritoneal space should already be developed for you. Additional blunt dissection may be necessary.
- Divide subcutaneous tissue and fascia, but do not breach peritoneum.
- Gently retract bladder out of the way
- *Note: If Foley in place and bladder decompressed, may not immediately visualize bladder, particularly if large hematoma is present. Proceed carefully.
- Pack the pelvis with three laparotomy pads on each side.
- If the pre-peritoneal dissection is difficult, the patient likely does not have a large pelvic hematoma… and another source of hemorrhage should be sought.
- If the pre-peritoneal dissection is difficult, the patient likely does not have a large pelvic hematoma… and another source of hemorrhage should be sought.
- Pelvic angioembolization:
- Activate STAT IR and Post Case for OR 41
- See STAT Interventional Radiology Consult Clinical Practice Policy.
- Trauma faculty to IR faculty direct discussion
- The IR team will meet you and the patient in the hybrid operating room for angiography.
- Activate STAT IR and Post Case for OR 41
Other operative Considerations ~
- Concomitant laparotomy is common when managing hemodynamically significant pelvic fractures.
- To preserve the pre-peritoneal space for packing, a skin bridge should be left between the PPP incision and the laparotomy incision.
- If performing a colostomy or suprapubic catheter, coordinate with orthopedic surgery as the location, as these can impact their pelvic fixation/reconstruction.
- Careful evaluation of the perineum needs to be performed in the emergency department and/or operating room so that open wounds are not missed.
Indications to Consider Emergent External Fixation:
- The pelvic binder provides adequate reduction of the pelvic ring in most cases.
- If access to the groin, abdomen, genitalia, or perineum is necessary and closure of the pelvic ring by wrapping the feet and/or moving the pelvic binder lower is unsuccessful, then discuss with orthopedic surgery regarding emergent external fixation.
References:
- Alton, T. B., & Gee, A. O. (2014). Classifications in brief: young and burgess classification of pelvic ring injuries. Clinical Orthopaedics and Related Research®, 472, 2338-2342.
- Brenner ML, Moore LJ, DuBose JJ, Tyson GH, McNutt MK, Albarado RP, Holcomb JB, Scalea TM, Rasmussen TE. A Clinical Series of Resuscitative Endovascular Balloon Occlusion of the Aorta for Hemorrhage Control and Resuscitation. J Trauma Acute Care Surg. 2013 Sep;75(3):506-11.
- Coccolini, F., Stahel, P. F., Montori, G., Biffl, W., Horer, T. M., Catena, F., … & Ansaloni, L. (2017). Pelvic trauma: WSES classification and guidelines. World Journal of Emergency Surgery, 12, 1-18.
- Cothren CC, Osborn PM, Moore EE, Morgan SJ, Johnson JL, Smith WR. Pre-peritoneal Pelvic Packing for Hemodynamically Unstable Pelvic Fractures: a Paradigm Shift. J Trauma. Apr 2007;62(4):834-39.
- Cullinane, D. C., Schiller, H. J., Zielinski, M. D., Bilaniuk, J. W., Collier, B. R., Como, J., … & Wynne, J. L. (2011). Eastern Association for the Surgery of Trauma practice management guidelines for hemorrhage in pelvic fracture—update and systematic review. Journal of Trauma and Acute Care Surgery, 71(6), 1850-1868.
- Smith, W. R., Moore, E. E., Osborn, P., Agudelo, J. F., Morgan, S. J., Parekh, A. A., & Cothren, C. (2005). Retroperitoneal packing as a resuscitation technique for hemodynamically unstable patients with pelvic fractures: report of two representative cases and a description of technique. Journal of Trauma and Acute Care Surgery, 59(6), 1510-1514.