Acute Care Surgery Pre-Operative NPO Protocol
Original Date: 03/2014 | Supersedes: 08/2017, 06/2021 | Last Review Date: 04/2024
Purpose: To safely minimize the amount of perioperative fasting in critically injured trauma patients.
This protocol applies to patients scheduled to go to the operating room or interventional radiology suite for a planned procedure.
Patients with a secured airway with a cuff (e.g. endotracheal tube, tracheostomy)
- When receiving gastric enteral feeds:
- The bedside nurse is to make the patient nothing per os (NPO) once the patient is called for the operating
- There will be no automatic NPO status after
- At the time the patient is called for the operating room, the bedside nurse will suction the stomach unless no orogastric/nasogastric tube (OGT/ NGT) is present, in which case an OGT will be inserted for this purpose (inserted intra-operatively by anesthesiologist).
- The volume of suctioned content is to be recorded in Care4 in the output section and based off of the volume recorded in the anesthesia record/handoff form.
- Common surgeries that should be NPO (this list is not intended to include all possibilities):
- Tracheostomy (or other procedures/surgeries involving the airway including tube changes)
- Patients undergoing procedures necessitating prone positioning such as:
- Posterior cervical spine
- Thoracic, lumbar spine
- Sacral procedures
- Video-assisted thoracoscopic surgery (VATS)
- Face and neck surgery
- Gastrostomy and jejunostomy
- If concerns are specifically raised by the OR (Anesthesiology or Surgery) team and documented preoperatively
- Common surgeries that should not be NPO (this list is not intended to include all possibilities):
- Rib plating
- Abdominal washout
- Orthopedic extremity procedures
- Plastic and/or reconstructive surgery on the extremities
- When receiving post-pyloric* enteral feeds
- Post-pyloric enteral feeds will be discontinued once the patient is called for the operating room
- There will be no automatic NPO status after midnight regardless of airway status
- *For patients with an unprotected airway, post-pyloric tube placement should be confirmed within 48 hours of procedure
- Patients without a secured airway with a cuff (e.g. not intubated, uncuffed tracheostomy):
- When receiving per os (PO) feeds
- MD orders clear liquid diet after midnight
- Bedside RN stops clear liquid diet 3 hours before the posted surgical time
- MD resumes previous diet after procedures
- When receiving gastric enteral feeds
- MD orders NPO after midnight
- Resume enteral nutrition at previous rate after procedures
- When receiving post-pyloric enteral feeds
- Post-pyloric enteral feeds will be discontinued once the patient is called for the operating room
- There will be no automatic NPO status after midnight regardless of airway status
- When NPO due to non-functional GI tract or other appropriate reasons
- Continue NPO order
- When receiving per os (PO) feeds
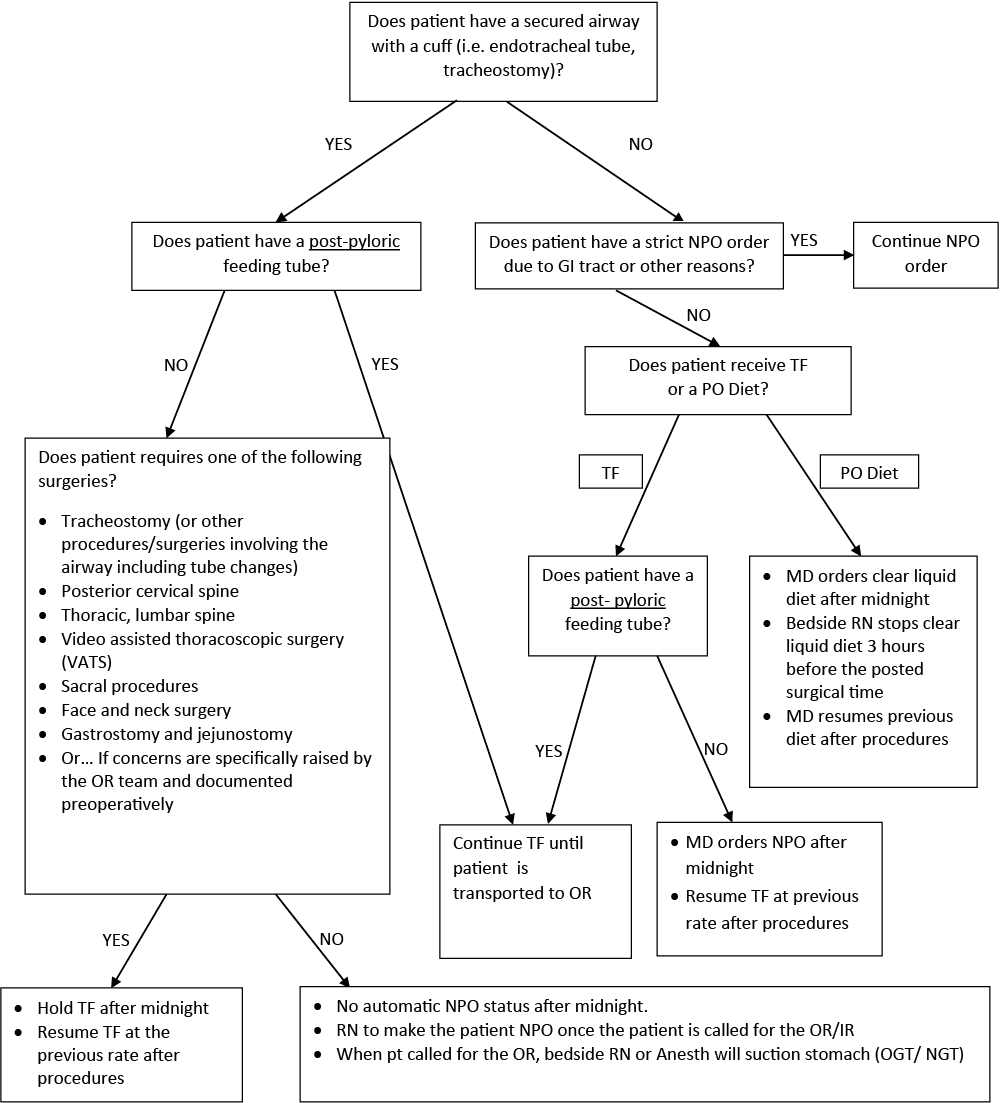
Pre-operative NPO Protocol Flowsheet
References
- Crenshaw JT, Winslow EH. Preoperative fasting: old habits die hard. Am J Nurs.2002 May;102(5):36-44
- Brady, M., Kinn, S., & Stuart, P. (2003). Preoperative fasting for adults to prevent perioperative complications. Cochrane Database of Systematic Reviews 2003, Issue 4. Art. No.:CD004423
- Pandit, S.K., Loberg, K.W., & Pandit, U.A. (2000). Toast and tea before elective surgery? A national survey on current practice. Anesthesia & Analgesia, 90, 1348-1351
- McKinley AC, James RL, Mims GR 3rd. NPO after midnight before elective surgery is no longer common practice for the majority of anesthesiologists. Am J Anesthesiol. 1995 Mar-Apr; 22(2):88-92
- Scarlett M, Crawford-Sykes A, Nelson M. Preoperative starvation and pulmonary aspiration. New perspective and guidelines. West Indian Med J. 2002 Dec; 51(4):241-5
- Change in “npo” policy reveals safety and increased caloric intake of enteral feedings at a level one trauma center. M McCunn, A Linton, S Clifton, TM Scalea, R Adams Cowley Shock Trauma Center, University of Maryland, Baltimore
- Lee, J.C., Williams, G.W., Kozar, R.A., Kao, L.S., Mueck, K.M., Emerald, A.D., Villegas, N.C., Moore, L.J. Multitargeted Feeding Strategies Improve Nutrition Outcome and Are Associated With Reduced Pneumonia in a Level 1 Trauma Intensive Care Unit. J Parenter Enteral Nutr.