Preventing and Correcting Hypothermia in Pediatric Trauma Patients
Original Date: 05/2013 | Supersedes: 05/2013, 06/2017, 09/2021 | Last Review Date: 02/2024 (Reviewed with no changes)
Purpose: The purpose of this clinical practice guideline is to establish guidance for prevention and management of hypothermia in pediatric trauma patients. We will track outcomes of hypothermic versus normothermic pediatric trauma patients that were admitted to the PICU/PIMU in subsequent 3 months from implementation of guideline. Additionally, we will compare outcomes of hypothermic patients before and after implementation of guideline.
Applicability/ Issue
- Increasing number of critically injured pediatric patients arriving in the PICU with initial documented temperatures in hypothermic range. This can lead to poor outcomes as well as increased length of stay, compounding medical management of patients.
Background
- In order to prevent hypothermia, situational awareness must be raised regarding the problem as well as proven preventative and treatment strategies.
- Hypothermia is a common finding among patients often complicating the management of those with severe penetrating or blunt trauma. Studies have shown that although permissive hypothermia in prehospital cardiac arrest patients can be protective for anoxic brain injury following resuscitation, incidence of secondary hypothermia associated with traumatic injuries and hemorrhagic shock can be fatal. Studies from Hutchison et al have shown that therapeutic hypothermia in pediatric patients with traumatic brain injury do not improve neurologic recovery and were associated with increased mortality.1Hypothermia in the trauma patient should be considered as a distinct entity from hypothermia induced by other causes. Mortality from moderate hypothermia (28°C–32°C) due to exposure is less than 25%, with virtually all deaths attributable to underlying diseases, rather than to hypothermia.3 In contrast, in trauma patients a core temperature less than 32°C was associated with 100% mortality, and any decrease in temperature below 35°C should be seen as a poor prognostic sign.2Unintentional hypothermia following traumatic injury represents a failure of the body’s compensatory mechanisms for thermoregulation. The body typically responds to heat loss by shivering, which increases metabolic demand and oxygen consumption in skeletal muscles anywhere from 40% – 400%; 6 this shift in increased demand puts some organs at risk for developing ischemia. In severe trauma, as hemorrhagic shock overwhelms the bodies’ compensatory mechanisms, anaerobic metabolism begins to develop. The resulting acidosis leads to coagulopathies that are compounded by the effects of hypothermia. Hypothermia has long been shown to be inhibitory toward the enzymatic rates of the coagulation cascade. Prolonged clotting times can occur with systemic depletion of clotting factors and diffuse coagulopathy occurs.Other studies show multiple other adverse effects of hypothermia especially in trauma, some of which include impaired cardiorespiratory function, cardiac depression, MI, impaired tissue oxygen delivery, increased risk of infection with decreased WBC numbers and function, and impaired cellular immune responses.5
Responsibilities
- Become familiar with the guidelines for prevention, monitoring, and management of hypothermia in pediatric trauma patient
Definitions
- Primary hypothermia occurs when heat production is normal, but body temperature decreases as a result of severe heat loss due to environmental conditions
- Secondary hypothermia is a result of diminished heat production. Body heat is generated as a result of oxygen consumption, and when oxygen consumption is pathologically reduced the result is a decrease in core temperature without severe environmental cold stressors
- Mild hypothermia (32–36°C) (90–96.8°F)
- Moderate hypothermia (28–32°C) (82–90°F)
- Severe hypothermia (20–28°C) (68–82°F)
Eligible Patients
- All pediatric Level 1 and 2 trauma patients admitted to the ED
- Outcomes will only be tracked for patients admitted to PICU and PIMU as they are the most critically injured and most likely to be harmed by hypothermia
Interventions and Sequential Management
- Identify potential reasons for hypothermia
- Primary versus secondary causes for hypothermia
- Interventions
- Normothermia – prevention of hypothermia
- Passive warming strategies
- Removal of the trauma patient from the cold environment (including external temperature, wet clothes/garments)
- Increasing the temperature in rooms
- Covering the patient with multiple warm blankets, especially in children/newborns, covering with caps and booties
- Aggressive measures encouraged
- Specialized equipment
- Convective (forced air warming) – Bair hugger
- These devices transfer heat across cutaneous surface as well as creation of thermoneutral microenvironments so that all heat production goes to restoring body temperature
- In a randomized controlled trial of hypothermic patients (with average core temperature of 28.8°C), forced-air warming increased core temperature by about 2.4°C per hour versus 1.4°C per hour in control patients. Both groups of patients received IV fluids warmed to 38°C as well as warmed, humidified oxygen at 40°C by inhalation4
- Convective (forced air warming) – Bair hugger
- Specialized equipment
- Passive warming strategies
- Hypothermia – any temperature <36 degrees
- Passive warming strategies as above
- Consideration that although passive interventions are effective, if a patient’s thermoregulatory mechanism is not intact, this strategy can still allow patients to cool
- Active Methods – More invasive means of rewarming patients involving specialized equipment
- Conductive garments: warm water garment — Arctic sun
- System to circulate warm water through a whole body garment to allow transferring of heat via conduction. Studies show that conduction is more effective than convection warming. The warm-water garment allows more body area to be covered and warmed than does the forced- air system.
- Artic sun will be used in place of Bair Hugger if already applied
- Intravenous fluids will be warm if given
- Blood products will be given through a fluid warmer (Belmont Buddy for <20 kg or Belmont for all others)
- Conductive garments: warm water garment — Arctic sun
- Passive warming strategies as above
- Normothermia – prevention of hypothermia
Summary
Unintentional hypothermia is a frequent complication of traumatic injury and significantly increases morbidity and mortality in these patients. Although initial normal temperatures are present, removal of the patient’s clothing, heat radiation through large open wounds and thermodilution with room temperature IV solutions all contribute to rapid heat loss.
Passive re-warming strategies are an effective first step on slowing the rate of deterioration, although these measures used in isolation are often insufficient to prevent hypothermia in severely injured patients. In those instances, active rewarming measures need to be taken to avoid harmful hypothermia.
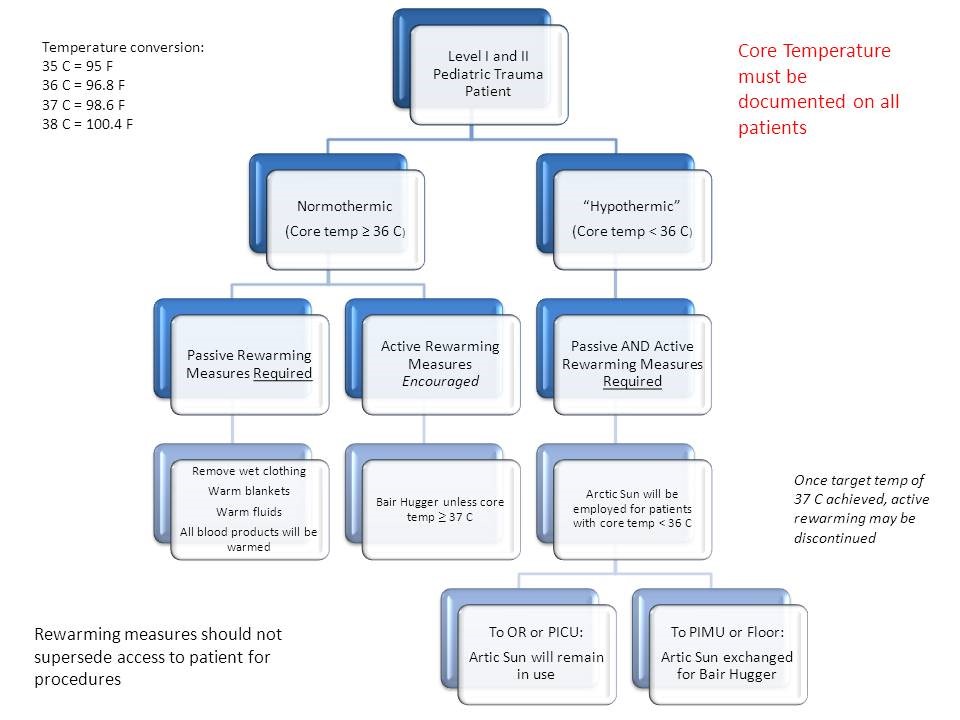
Algorithm
References
- Hutchison J.S, Ward R. Hypothermia Therapy after Traumatic Brain injury in Children; N Engl J Med 2008; 358:2447-56.
- Gentilello L, Pierson D. Trauma critical care. Am J Respiratory Critical Care Med. 2001; 163: 604-607.
- Helm M, Lamp L, Hauke J, Brock K. Accidental hypothermia in trauma patients. Is it relevant to preclinical treatment? Anesthetist 1995; 44: 101-107.
- Smith C, Treatment and prevention of hypothermia in Trauma patients; The International Trauma and Anesthesia Critical Care Society, Spring 2004 Guidelines.
- Pavlin EG. Hypothermia in traumatized patients. In: Grande C, ed. Textbook of Trauma Anesthesia and Critical Care. New York: Mosby Year Book, 1993:1131–9.
- Luna GK, Maier RV, Pavlin EG, et al. Incidence and effect of hypothermia in seriously injured patients. J Trauma 1987; 27:1014–8.
- Gentilello LM, Jurkovich GJ: Hypothermia. In Ivatory RR, Cayten CG (eds.): The Textbook of Penetrating Trauma. Media, PA: Williams and Wilkins, 1996, pp 995–1006.