Snake Bites
Original Date: 07/2003 | Last Review Date: 05/2024
Purpose: To provide guidance on the evaluation and management of snake bites in the Houston area
Rattlesnake, Copperhead, and Water Moccasin Disposition
- If admission is warranted, consult appropriate hospitalist service for admission. Trauma or pediatric surgery should be consulted only if concern for compartment syndrome.
- Documented or concern for compartment syndrome should be admitted to Trauma/Pediatric Trauma with Hand subspecialty service consult as needed.
- If no concern for compartment syndrome after consultation, patient may be admitted to appropriate hospitalist service with surgical consultant(s).
- The following patients should be placed in the ICU or IMU per discretion of the ED physician and/or hospitalist.
- Patients with systemic symptoms even if the symptoms resolved with the administration of antivenin.
- Patients with active bleeding and coagulopathy.
- Patients with grossly abnormal coagulation indices.
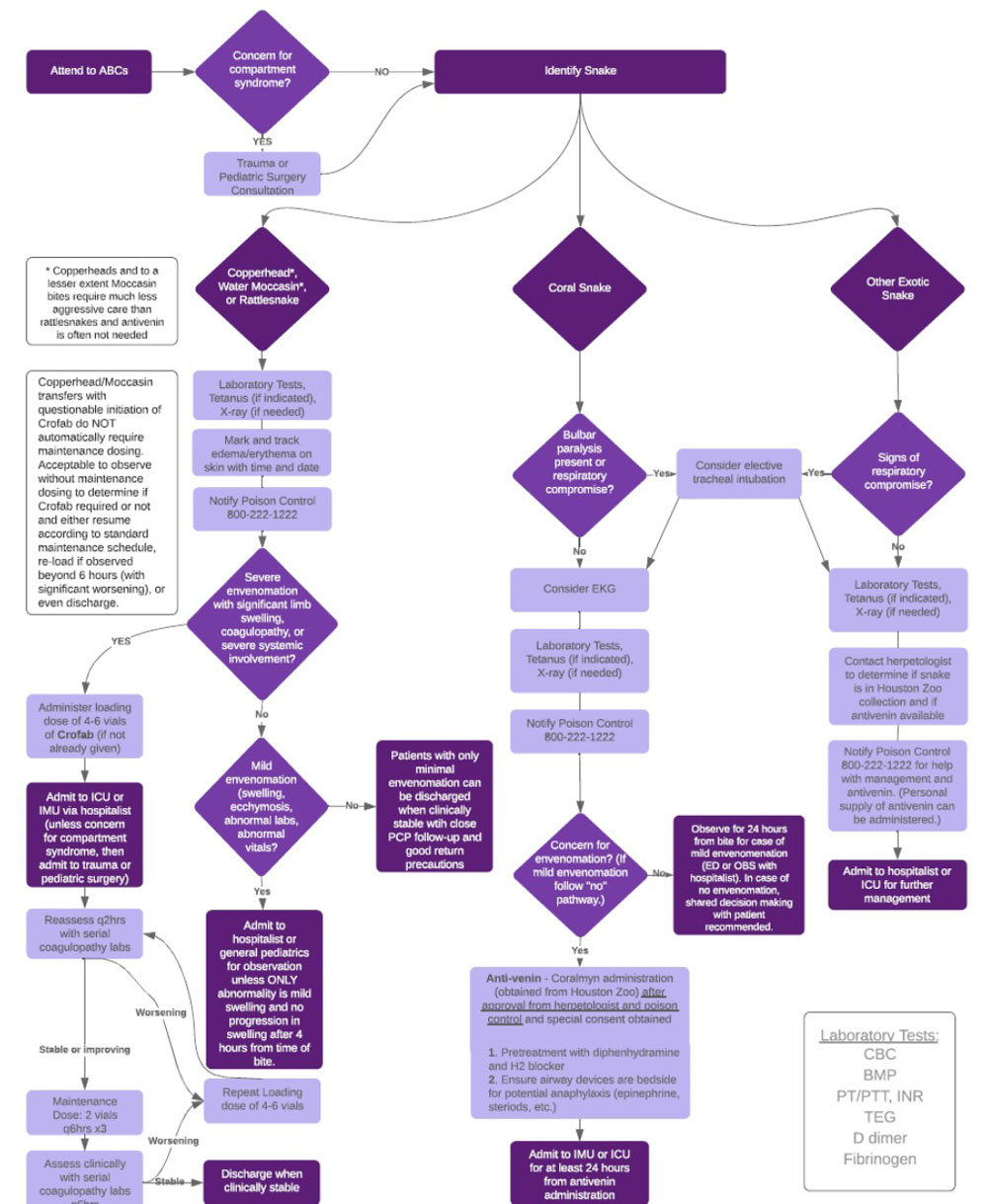
See below “Algorithm for Poisonous Snake Bite Management and Disposition” for full details.
Algorithm for Poisonous Snake Bite Management and Disposition