Soft Tissue Infections Requiring Hospitalization
Original Date: 02/2016 | Supersedes: Original 2016 | Last Review Date: 04/2022
Purpose: To decrease Interventional Radiology response time for critically injured patients.
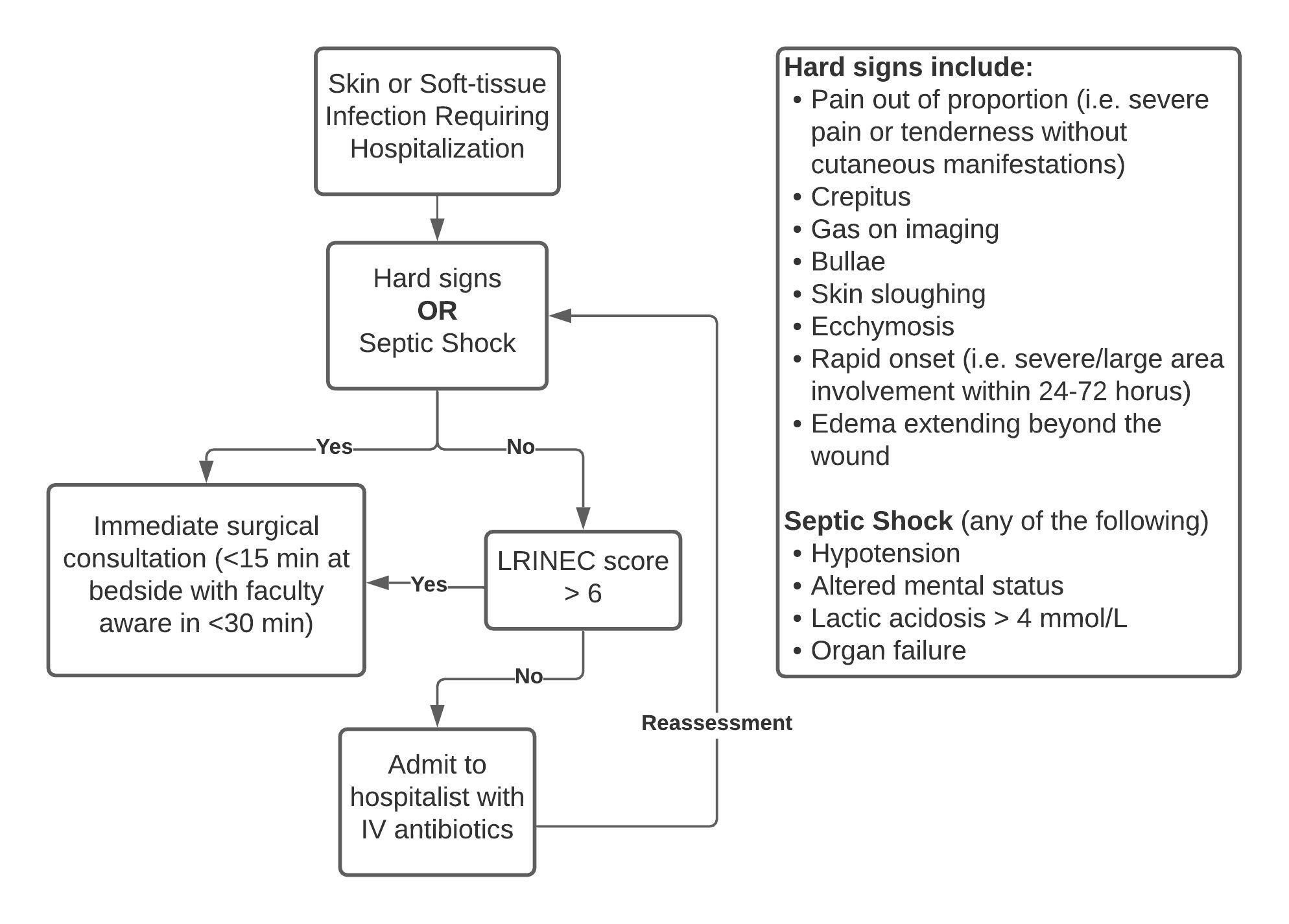
Purpose Statement: To revise current recommendations and help appropriately triage adult patients requiring hospitalization for cellulitis and/or suspected necrotizing infections.
Background: Necrotizing infections are surgical emergencies and early diagnosis is key to prevention of mortality, which can exceed 70%.1 Prior pathways for diagnosis relied heavily on the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score.2 A recent study by Hsiao et al. looked at 825 patients in the emergency department and calculated a sensitivity of 43% (95% CI 0.34-0.53), specificity of 83% (95% CI 0.8-0.86), positive predictive value of 25% (95% CI 0.2-0.3), negative predictive value was 92% (95% CI 0.91-0.93) when the cutoff was a score of >6.3 Specific parts of the LRINEC score do tend to be stronger predictors: WBC >15.4 or Na < 134 for example. Based on poor test characteristics, we believe that reliance on the LRINEC score will lead to misdiagnosis, and that greater emphasis on clinical information will improve diagnostic ability.
It is important to recognize the different sub-types of necrotizing infections to avoid common diagnostic pitfalls. Type I necrotizing fasciitis is a polymicrobial infection involving aerobic and anaerobic organisms. It is usually seen in the elderly and diabetics and is often associated with tissue gas. It usually involves a portal of entry and can have an indolent course. Type II necrotizing fasciitis is monomicrobial (often s. pyogenes) and can involve any age group including those without underlying illness. Type II infections are difficult to recognize because they often involve deep spaces that are seeded as a result of local inflammation and transient bacteremia often from trauma. Type II infections do not need a portal of entry and skin findings are late. These patients often have pain out of proportion – absence of external findings in a patient with severe pain or tenderness. Therefore, reliance on cutaneous manifestations is a common pitfall.1
Guideline: Patients presenting with hard signs (as defined below) or signs of septic shock (as defined below) warrant an emergent surgical consultation without delay.
Hard Signs of Necrotizing Infections Warranting Immediate Surgical Consultation
- Pain out of proportion (i.e. severe pain or tenderness without cutaneous manifestations)
- Crepitus
- Gas on imaging
- Bullae
- Skin sloughing
- Ecchymosis
- Rapid onset (i.e. severe/large area involvement within 24-72 hours)
- Edema extending beyond the wound
All patients requiring hospitalization for skin or soft-tissue infections may be further risk stratified with the LRINEC score according to the algorithm below.4
Special circumstances: Infections involving specialized areas might be better served by a surgical subspecialist.
- On-call hand service for infections involving the hand or forearm
- Oral maxillofacial surgery service for Ludwig’s angina
- Urology for Fournier’s gangrene
If any concern for involvement beyond usual anatomic cut-offs or patients with unclear anatomic demarcation, then a simultaneous consultation with EGS is recommended. Delays > 30 minutes must be escalated to on-call faculty.
Antibiotic Therapy Guide5
- Broad therapy covering for gram positives, negatives and anaerobes.
- Gram + coverage for MRSA with vancomycin, daptomycin or linezolid, PLUS
- (1) Ceftriaxone/cefepime plus metronidazole, or
- (2) Piperacillin-tazobactam, or
- (3) a carbapenem (imipenem-cilastatin, meropenem, and ertapenem), or
- (4) a fluoroquinolone plus metronidazole
- The addition of clindamycin is recommended when there is a strong suspicion for Group A Streptococcus or Toxic Shock Syndrome.
- Gram + coverage for MRSA with vancomycin, daptomycin or linezolid, PLUS
References
- Stevens DL, Bryant AE. Necrotizing Soft-Tissue Infections. Longo DL, ed. The New England journal of medicine. 2017;377(23):2253-2265. doi:10.1056/NEJMra1600673
- CH W, LW K, KS H, KC T, CO L. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Critical care medicine. 2004;32(7):1535-1541. doi:10.1097/01.CCM.0000129486.35458.7D
- Hsiao C-T, Chang C-P, Huang T-Y, Chen Y-C, Fann W-C. Prospective Validation of the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) Score for Necrotizing Fasciitis of the Extremities. PLOS ONE. 2020;15(1):e0227748. doi:10.1371/JOURNAL.PONE.0227748
- L S, DE N. Using clinical pathways to aid in the diagnosis of necrotizing soft tissue infections synthesis of evidence. Worldviews on evidence-based nursing. 2012;9(2):88-99. doi:10.1111/J.1741-6787.2011.00235.X
- DL S, AL B, HF C, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2014;59(2):147-159. doi:10.1093/CID/CIU444