STICU ARDS Algorithm
Original Date: 10/2019 | Last Review Date: 4/2023
Purpose: To delineate the management of patients with acute respiratory distress syndrome (ARDS)
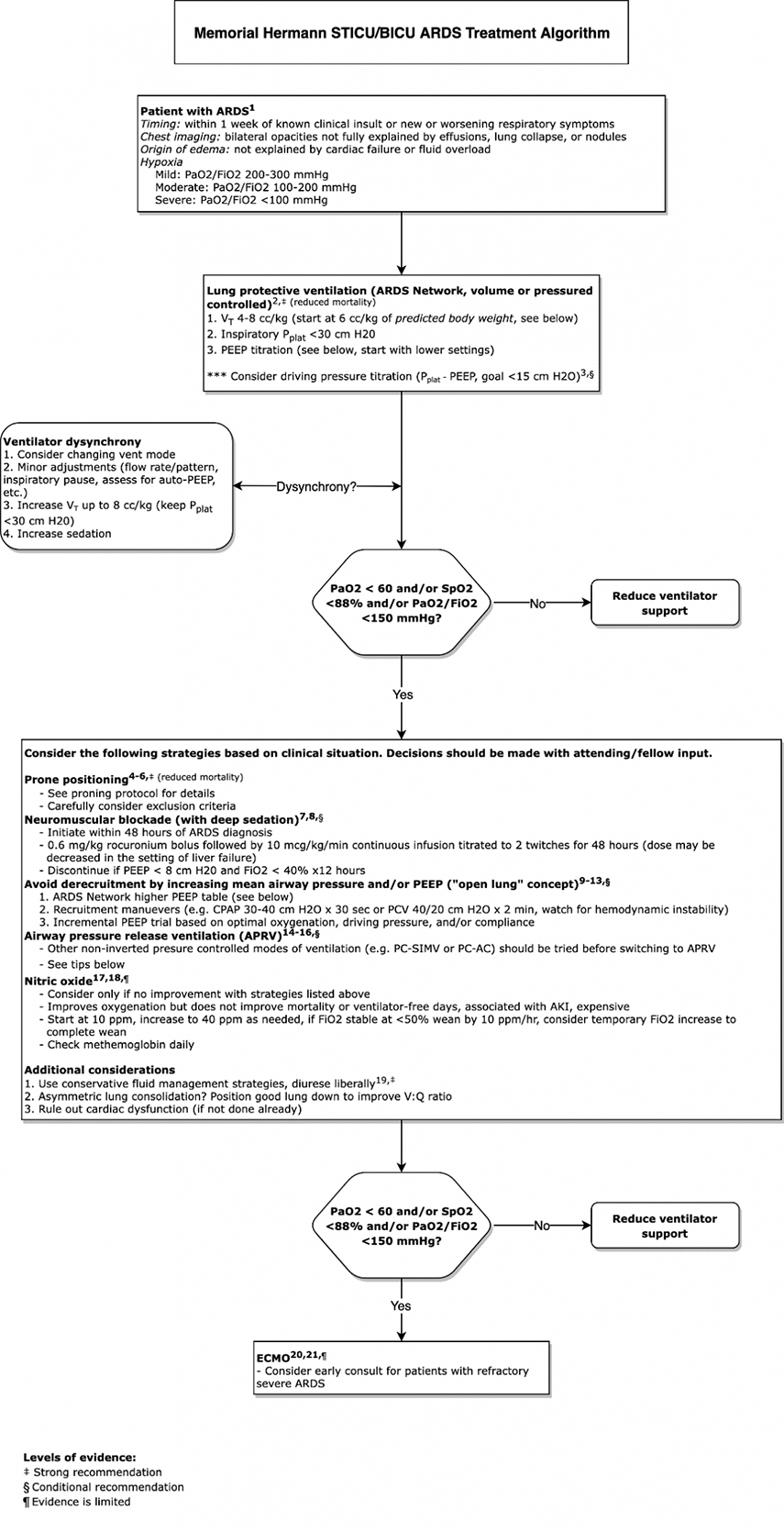
APRV tips
- APRV is an inverse ratio pressure control type setting (designated as Bi-Level PC/PS on Puritan Bennett 980 ventilator)
- Set PHigh (use desired plateau pressure, typically 25-30 cm H2O)
- Set PLow (default = 3 cm H2O)
- Set TLow to create desired auto-PEEP and VT
- Auto-PEEP is created by cutting expiration short
- TLow typically 0.2-0.8 sec (0.8 sec is good starting point)
- Observe expiratory flow graphic to target an expiratory flow cutoff of 50-75% of peak expiratory flow
- Assess auto-PEEP (via an expiratory hold) and adjust TLow/expiratory flow cutoff to achieve desired auto-PEEP
- Assess VT (goal ~ 6 cc/kg predicted bodyweight) and adjust TLow/expiratory flow cutoff to achieve desired VT
- Set respiratory rate (typically 10-15/min). This is the easiest way to manipulate THigh and the I:E ratio.
References
- The ARDS Definition Task Force. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA.2012;307(23):2526–2533 {ARDS definition}
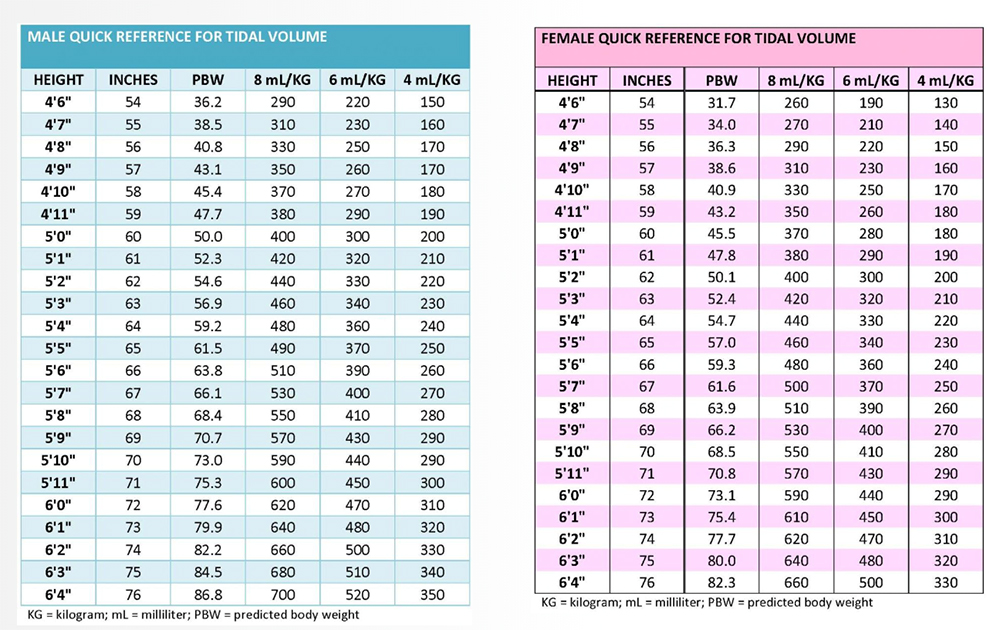
- The ARDS Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. NEJM.2000;342(19):1301-1308 {Seminal RCT, showed reduced mortality with VT <6 cc/kg predicted body weight and PPlat < 30 cm H2O}
- Amato MB, et al. Driving pressure and survival in the acute respiratory distress syndrome. NEJM.2015;372:747–55 {Secondary analysis of data from 9 RCTs showing driving pressure more strongly associated with survival than VT and PPlat}
- Guerin C, et al. Prone Positioning in Severe Acute Respiratory Distress Syndrome. NEJM.2013;368:2159-2168 {RCT, showed prolonged (>16 hr/day) early (<48 hrs after diagnosis) proning decreases mortality in ARDS patients with P/F <150}
- Bloomfield R, et al. Prone Position for Acute Respiratory Failure in Adults. Cochrane Database Syst Rev.2015;Nov 13(11):CD008095 {Cochrane review showing early, prolonged proning in moderate-severe ARDS may improve mortality}
- Dickenson et al. Prone Positioning Therapy in ARDS. Crit Care Clin.2011;27:511-523 {Review with practical tips for proning}
- Papazian et al. Neuromuscular Blockers in Early Acute Respiratory Distress Syndrome. NEJM.2010;363:1107-1116 {ACURASYS RCT, early administration of NMB decreased mortality and ventilator time without causing weakness in ARDS patients with P/F <150}
- The PETAL Network. Early Neuromuscular Blockade in Acute Respiratory Distress Syndrome. NEJM.2019;380:1997-2008 {ROSE RCT, early administration of NMB did NOT decrease mortality in ARDS patients with P/F <150}
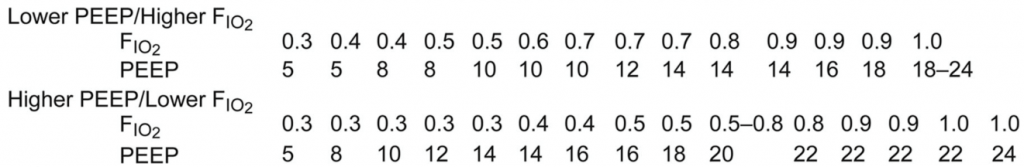
- Briel M, et al. Higher vs Lower Positive End-Expiratory Pressure in Patients with Acute Lung Injury and Acute Respiratory Distress Syndrome: Systematic Review and Meta-Analysis. JAMA.2010;303:865–873 {Secondary analysis of data from 9 RCTs showing decreased mortality in ARDS patients with P/F < 200 treated with higher PEEP}
- Cavalcanti AB, et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs. Low PEEP on Mortality in Patients with Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA. 2017;318:1335–45 {ART RCT, showed increased mortality in ARDS patients with P/F <200 managed with recruitment maneuvers and PEEP titration}
- Van der Zee, et al. Recruitment Maneuvers and Higher PEEP, the So-Called Open Lung Concept, in Patients with ARDS. Crit Care. 2019;23(1):73 {Review of the open lung concept including recruitment maneuvers and PEEP}
- Bhattacharjee S, et al. Recruitment Maneuver Does Not Provide Any Mortality Benefit Over Lung Protective Strategy Ventilation in Adult Patients with Acute Respiratory Distress Syndrome: A Meta-Analysis and Systematic Review of the Randomized Controlled Trials. J Intensive Care. 2018;6:35 {Secondary analysis of data from 7 RCTs showing no improvement in mortality in ARDS patients treated with recruitment maneuvers}
- Hess D. Recruitment Maneuvers and PEEP Titration. Respir Care. 2015;60:1688-1704 {Comprehensive review of recruitment maneuvers and PEEP}
- Habashi NM. Other approaches to open-lung ventilation: airway pressure release ventilation. Crit Care Med. 2005; 33(Suppl): S228-S240 {Seminal review of APRV, including how to set up}
- Zhou Y, et al. Early Application of Airway Pressure Release Ventilation May Reduce the Duration of Mechanical Ventilation in Acute Respiratory Distress Syndrome. Intensive Care Med. 2017;43:1648-1659 {RCT, early APRV increased days free from ventilator and oxygenation and decreased PPlat}
- Carsetti et al. Airway Pressure Release Ventilation During Acute Hypoxemic Respiratory Failure: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ann Intensive Care. 2019;9(1):44 {Secondary review of 5 RCTs showing lower mortality and increased days free from ventilator in ARDS patients treated with APRV}
- Gebistorf F, et al. Inhaled Nitric Oxide for Acute Respiratory Distress Syndrome (ARDS) in Children and Adults. Cochrane Database Syst Rev. 2016 Jun 27;(6):CD002787 {Cochrane review showing NO improves oxygenation but not mortality and may cause kidney injury}
- Adhikari NK, et al. Inhaled Nitric Oxide Does Not Reduce Mortality in Patients With Acute Respiratory Distress Syndrome Regardless of Severity: Systematic Review and Meta-Analysis. Crit Care Med. 2014;42(2):404-412 {Secondary review of 9 RCTs showing NO does not improvement in mortality}
- The ARDS Network. Comparison of Two Fluid-Management Strategies in Acute Lung Injury, NEJM. 2006;354:2564-2575 {RCT, conservative fluid management strategy increased days free from ventilator, mean difference of 7 liters over 7 days}
- Peek G, et al. CESAR: Efficacy and Economic Assessment of Conventional Ventilatory Support Versus Extracorporeal Membrane Oxygenation for Severe Adult Respiratory Failure. A Multicenter Randomised Controlled Trial. Lancet. 2009;374:1351-1363 {CESAR RCT, showed that transfer to an ECMO center improved mortality, does NOT necessarily show that ECMO is superior to lung protective ventilation, only ¾ of patients randomized to ECMO went on}
- Combes A, et al. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome. NEJM. 2018;378:1965-1975 {EOLIA RCT, in patients with very severe ARDS no statistically significant mortality difference with ECMO (35 vs. 46%, p=0.09), crossover to ECMO in 28% in control group}
* Thank you to the University of Michigan Respiratory Care Committee for sharing resources and expertise that were used to help make this algorithm