Trauma Team Activation for Pediatrics (age 15 years and below)
Original Date: 9/2000 | Supersedes: 08/2005, 04/2008, 7/2008, 05/2009, 04/2011, 08/2011, 05/2012, 08/2012, 11/2012, 04/2013, 08/2013, 12/2016, 6/2020, 10/2020, 10/2021 | Last Review Date: 03/2024
Purpose: Patients who are critically injured by trauma require rapid assessment and intervention using a team approach. This guideline is to provide consistent guidelines for the identification of patients who require a trauma team activation and timely notification of appropriate team members.
Procedure: Injured patients will be categorized and given a level based on criteria in this guideline.
- The trauma team will be group paged using TraumaPage software from a PC terminal in one of three locations: Emergency Center Triage, Life Flight Dispatch, and Emergency Center Trauma resuscitation area. The following information is required to determine the appropriate level of response.
- Patient’s approximate age, gender, ETA to Memorial Hermann Hospital, GCS, systolic blood pressure, respiratory rate, pulse and mechanism of injury
- Anatomical findings
- Mechanism of injury
The TraumaPage software program will determine the appropriate level of response and automatically page the appropriate team members.
In the event of a malfunction of the TraumaPage software or associated computer hardware, the support center will be notified of the issue. The following process will be used to notify the trauma team of patient’s arrival:
-
- The Life Flight communications office will notify the emergency center charge nurse and identify to them that the TraumaPage system is not working and relay information above on the incoming trauma patient including the level.
- The emergency center charge nurse will notify the trauma EC attending and the Trauma Chief. The Trauma Chief will notify the Trauma Attending.
- Tiered response for Pediatrics – the following criteria will be used to determine the level of activation required for patients care age 15 years and below.
| Response Tier | Criteria | Personnel |
|---|---|---|
| Level 1 (Most Severe Injuries) |
Physiologic Criteria – criteria indicating high risk or life threatening injuries including any of the following:
Anatomic Criteria – criteria indicating high risk or life threatening injuries including any of the following:
|
Response Team Trauma Attending Trauma PGY 4-5 Trauma PGY 2 Trauma PGY 1 Pedi Surgery Resident EM Attending EM PGY 2/3 EM PGY 1 EC RN x2 Radiology Resident Radiology Tech Respiratory Tech Trauma Medical Students Also Notified |
| Level 2 (Moderate Injuries) |
None of the above findings and any of the following:
|
Response Team EM Attending EM PGY 2/3 EM PGY 1 EC RN x2 Radiology Tech Also Notified |
| Urgent Consult |
|
Response Team Pedi Trauma Attending Pedi Trauma Fellow |
Trauma Team Roles and Response
- Pediatric Trauma Integrated First Response:
- The adult trauma attending surgeon is the immediate responder for pediatric level one trauma patients.
- The adult trauma attending surgeon is responsible as the team leader for the primary/secondary survey and initiation of resuscitative interventions.
- The adult trauma attending surgeon will document on the trauma H&P or consult as appropriate.
- The patient is then handed-off to the pediatric surgery team. Depending on the acuity of the patient, this may be an APSP, HO or Pediatric Attending Surgeon.
- Life/limb threatening injuries requiring surgical management can proceed to the OR with the adult trauma attending surgeon if necessary, while the pediatric attending surgeon is en route.
- The pediatric surgery attending/fellow/PGY4 will evaluate all patients going to OR pre-operatively/meet in OR (for procedures that trauma attending is primary) for evolving and unstable patients. PICU admissions with multi-system injury will be evaluated within 2-6 hours depending on acuity. Isolated injures requiring ICU admission will be evaluated by the surgical service for the primary injury within 2-6 hours depending on acuity of patient.
- Urgent consults will be evaluated by pediatric surgery attending/fellow within 6 hours.
- Non-urgent or none ICU admissions will be seen by a pediatric trauma provider within 6 hours of consult.
- The pediatric surgery attending is the admitting physician of record regardless of the unit of admission.
- General Pre-arrival Preparation
- All trauma team members who anticipate direct patient contact
- Assume a protective gown, gloves, shoe coverings, protective mask, goggles or glasses, and head cover
- Assemble in the assigned resuscitation room and sign in on time out board. Assume assigned position and state their name and role to the nurse recorder
- Physician Staff
- Trauma team leader will assign specific roles and tasks to available physicians and medical students
- Nursing Staff
- Bring in trauma cart
- Ensure Belmont infuser is in room, ready and accessible
- Prepare specimen collecting supplies
- Trauma Technician
- Responds to blood bank on patients arriving with blood infusing prior to arrival and brings the initial cooler of products
- Radiology Staff
- Respond to Trauma Team Code
- Ensures requested images are ordered in the computer
- Completes requested images
- All trauma team members who anticipate direct patient contact
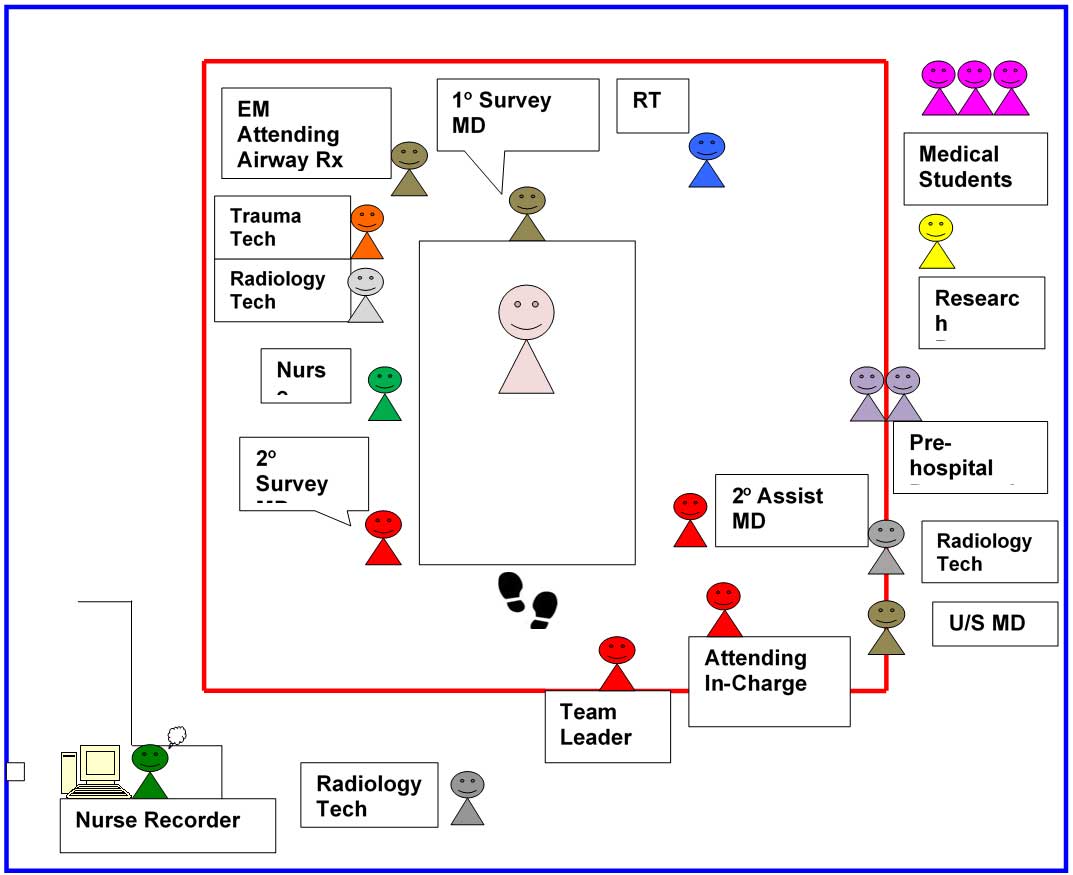
Arrival Management (See diagram for positions in trauma room)
- Pre-hospital Personnel
- Gives report while patient is moved to the trauma stretcher
- EMS and Hospital staff move patient to trauma stretcher
- Attending in Charge/Team leader (Trauma and/or EM physician if trauma not present)
- Utilize ATLS guidelines to supervise primary survey, secondary survey and resuscitative measures as deemed necessary
- Assume responsibility for the evaluation and management of the injured patient until transfer of care to the appropriate service attending or until discharge of the patient from the emergency center
- Maintain open and active communication with the trauma team leader
- Authorize consultations to specialty services
- Review and supervise the documentation of evaluation and management of care
- Facilitate the work up by reviewing radiology films as they become available
- Limits the number of people at the bedside to only those who are essential for initial evaluation, management and direct authorized observers to remain outside the designated trauma evaluation space
- Communicate directly to team
- Primary Survey (EC MD head of bed)
- Perform a rapid primary survey
- Identify the need for difficult airway cart
- Perform procedures as directed by the team leader
- Secondary Survey (Trauma Team MD Member left side of bed-facing patient)
- Assist in exposing the patient
- Perform secondary survey
- Perform assigned procedures and task
- Secondary Assist (Trauma Team MD Member right side of bed facing patient)
- Assist with exposing the patient
- Do task as directed by team leader
- RN (Recorder)
- Documents care on trauma template
- Document arrival times & names of trauma team
- Receive and document report from pre-hospital personnel or triage RN including mechanism of injury, GCS, assessment, physical findings, interventions, medications, type and volume given
- Document all findings during primary and secondary assessment
- Document fluids, blood and medications as announced
- Complete patient documentation
- Assure ICU, IR, or floor is notified with patient report and estimated time of arrival
- Document vital signs and neurologic status as clinically indicated and with any significant changes
- RN (Circulating RN)
- Obtains initial B/P manually and ensures collection of vital signs including a temperature in the initial set
- Obtain large bore peripheral IV access and blood samples
- Ensures recorder RN aware of all interventions and procedures performed
- Administer medications ordered by the trauma team leader
- Announce amount of crystalloid and blood products infused
- Trauma Technician
- Announces the initial cooler of products arrival
- Ensure that previous patient is discharged from monitor
- Place monitor leads on patient
- Ensure patient remains covered with warm blankets after secondary survey and resuscitation measures
- Deliver blood sample to lab and to blood bank and announces “Trauma team activation level 1”
- Patient Access
- Register patient
- Confirms Life Flight ID number
- Documents patients valuables on inventory list and places a copy of the inventory list with patient chart
- Charge RN
- Ensures and coordinates availability of beds
- Assist to facilitate a smooth and prompt transfer our of EC
- Radiology Tech
- Obtain images requested by trauma team leader
- Assist the team leader or assigned member in arranging for all subsequent radiological studies
- Radiology Resident/ Fellow/ Attending
- Be available to evaluate x-rays and CT scans as soon as they are processed and provide a prompt report in PACS
- Notify trauma team leader of any changes between the preliminary and the final report
- Provides final interpretation of screening CT scans (head, C- spine, CAP) within 12 hours
- Respiratory Therapy
- Ensure ETT is secure after handoff of airway management
- Make adjustments as instructed after imaging
- Manage ventilator and hand bagging as required
- Ultrasound Resident
- Perform F.A.S.T. ultrasound and announces findings
Trauma Team Roles