Advances in the Diagnosis & Management of Cluster Headache

Cluster headache frequently is described as the most excruciatingly painful of all headache disorders. For most patients, a cluster headache begins with a severe stabbing and burning pain on one side of the head, typically behind and around the eye, with a duration of 15 to 180 minutes. They occur in clusters, with bouts of frequent attacks – up to eight in a day – that last from weeks to months.
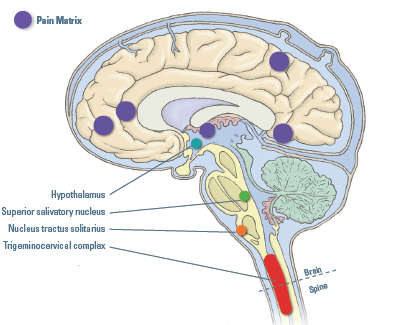
Based on clinical, imaging, biomarker, and neuromodulation studies, several systems and multiple brain areas are involved in cluster headache, according to our current understanding of their pathogenesis. Ultimately, these systems lead to activation of the widely distributed pain matrix (shown in purple). During a cluster headache attack, altered pain matrix areas include (from left to right in purple) the prefrontal cortex, anterior cingulate cortex, thalamus primary somatosensory cortex, and insula.
“Cluster headaches are violent, and patients are known to rock, pace, vocalize, or bang their head against a wall during an attack. Many have thoughts of suicide, and despite all this, accurate diagnosis often is delayed for years because the headaches are confused with migraines or trigeminal neuralgia,” says neurologist Mark Burish, MD, PhD, associate professor in the Vivian L. Smith Department of Neurosurgery and director of the Will Erwin Headache Research Center at McGovern Medical School at UTHealth Houston. Burish is also a faculty member of The University of Texas MD Anderson Cancer Center UTHealth Houston Graduate School of Biomedical Sciences. In 2022, Burish published an invited clinical review covering the clinical, pathophysiologic, and therapeutic features of cluster headache in The BMJ.1
The article is the first to include a video of a patient experiencing an acute cluster headache attack, and he classes it as “one of the 10 must-read articles of the year for all headache specialists as part of their annual continuing education requirements.” Since then, he has published invited clinical reviews in Cephalalgia,2 a journal for headache specialists, and Continuum,3 a journal for general neurologists.
“Our research goal was to improve understanding of the disease and advance treatment by detailing relevant pathophysiology and neuropharmacology. We also provided an update on available treatments,” he says. The clinical reviewers searched Medline for articles on cluster headache published during the last five years and reviewed them independently.
Key points made in the article include: Onset can occur at any age but typically is between ages 20 and 40; cluster headache is associated with an increased risk of sleep apnea; psychological comorbidities are common in patients, especially anxiety and depression; 55% to 64% of patients experience suicidal ideation, according to studies from the United States and South Korea; the best established comorbidity may be tobacco use; and the most common trigger appears to be alcohol use, present in 40% to 80% of patients. Previously, it was thought that men were more likely than women to have cluster headache, although the true gender ratio is unclear due to possible past misdiagnoses in women.
In a retrospective online survey of 1,604 patients with cluster headache, the average pain intensity was rated at 9.7 on a 0-10 point scale; the next highest pain rating was childbirth at 7.2.
“Our present understanding of cluster headache is based on clinical observations, molecular changes, and imaging findings,” Burish says. “Although the mechanism of cluster headache has not been fully explained, these suggest that the trigeminovascular system, the autonomic system, and the hypothalamus are involved.”
Acute treatments for cluster headache include subcutaneous sumatriptan and oxygen, both of which have limitations. Neurostimulation through a wearable vagus nerve stimulator (VNS) has been shown in clinical trials to stop attacks in patients with episodic cluster headache, but not in patients with chronic cluster headache.
New treatments for episodic cluster headache also include monthly injections with galcanezumab, a humanized monoclonal antibody used for the prevention of migraine. “With these new treatments available, early and accurate diagnosis is important,” Burish says.
References
1Schindler EAD, Burish MJ. Recent advances in the diagnosis and management of cluster headache. BMJ. 2022 Mar 16;376:e059577.
2Burish M. Cluster Headache, SUNCT, and SUNA. Continuum (Minneap Minn). 2024 Apr 1;30(2):391-410.
3Peng KP, Burish MJ. Management of cluster headache: Treatments and their mechanisms. Cephalalgia. 2023 Aug;43(8):3331024231196808.
In This Section:
Features:
- True to Our Values
- The Heart-Brain Program: A Closed-Loop Continuum of Care to Patients with PFO-Associated Stroke
- Multidisciplinary Programs Provide Convenience and a Broader View of Health to Physicians and Patients
Patient Stories:
- Alabama Woman Finally Gets a Sleep Disorder Diagnosis Through Telehealth
- Radiofrequency Ablation (RFA) for severe back pain
- Finally Getting a Good Night’s Sleep with remedē®
- Making a Difference by Participating in Huntington’s Disease Research
Research & Trials:
- Sensitizing Tumors to Radiation Therapy Using Gold Nanoparticles
- An Investigation: Th-1 Dendritic Cell Immunotherapy in Combination with Standard Chemoradiation for Adjuvant Treatment of Adult Glioblastoma
- Advances in the Diagnosis and Management of Cluster Headache
- AI-Powered Algorithms May Help Detect Unruptured Brain Aneurysms
Accolades & News:
- Department of Neurosurgery Ranks 4th in NIH Funding Among US Clinical Science Departments
- McCullough Wins Stroke Association Lecture Award
- UTMOVE Receives Distinguished Edmond J. Safra Fellowship in Movement Disorders
- Schiess Awarded UTHealth Houston President’s Scholar Award
- Burish Co-Chairs the AHS Scientific Program Committee
- Furr Stimming Named HSG Outstanding Investigator
- Lo Receives UT System STARs Award
- Burish Assumes Responsibility for Neurology Residency Training for Headache Medicine
- Morcos Named Chair of Neurosurgery











