Skin Cancer Reconstruction
When skin cancer is removed, especially through Mohs micrographic surgery—a precise technique used to excise cancerous tissue layer by layer—reconstruction is a vital step to restore both appearance and function. The goal of skin cancer reconstruction is to achieve the most natural and aesthetically pleasing result possible while preserving the functional integrity of facial subunits such as the eyelids, nose, lips, and ears.
Why Reconstruction Is Important
Skin cancer removal often leaves defects in delicate and highly visible areas. These defects vary in size, depth, and location, making personalized reconstruction necessary to: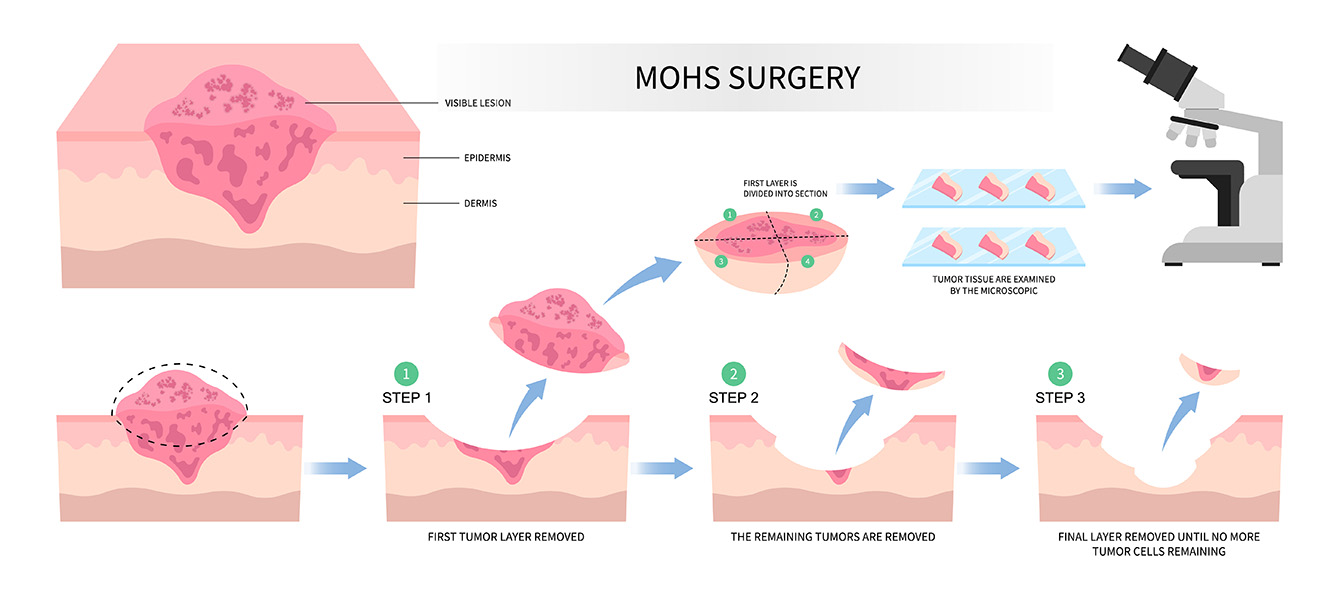
- Restore normal appearance,
- Preserve facial movements and functions (e.g., blinking, speaking, breathing),
- Minimize scarring and deformity,
- Promote optimal wound healing.
Reconstruction Techniques
There are several surgical options available, each tailored to the specific characteristics of the defect and surrounding tissues. The reconstructive surgeon will consider these factors to choose the best approach:
- Primary Closure: Simple suturing of the wound edges, used for small defects with sufficient surrounding laxity.
- Skin Grafts: Transplanting a piece of skin from another area to cover the defect; often used for larger wounds or areas with insufficient surrounding tissue.
- Local Flaps: Moving adjacent tissue to cover the wound while maintaining its blood supply. These flaps can contour well and often yield superior cosmetic results.
- Regional or Distant Flaps: For large or complex defects, tissue from other parts of the body may be used.
- Complex Reconstruction: Involving multiple techniques or staged procedures for extensive defects.
Considerations in Reconstruction
Each facial subunit has specific functional and aesthetic roles. For example:
- Eyelids: Critical for eye protection and lubrication; reconstruction must preserve movement.
- Nose: Central facial feature with unique contours; reconstruction requires attention to shape and airway.
- Lips: Essential for speech, eating, and expression; restore both form and muscular function.
The surgeon’s expertise in these nuances ensures that reconstruction supports both appearance and daily function.
Treatment Settings
Reconstruction can be performed:
- In-office: For smaller and less complex defects, offering convenience and quicker recovery.
- Surgical Center or Hospital: For larger or complex reconstructions requiring anesthesia and specialized equipment.
Advancements in Skin Cancer Reconstruction
Recent guidelines from leading societies, such as the American Society of Plastic Surgeons and the American Society for Dermatologic Surgery, emphasize evidence-based approaches to optimize outcomes. Innovations include improved flap designs, advanced suturing techniques, and new biomaterials that enhance healing and aesthetics.
Patient-Centered Care
We prioritize individualized treatment planning, thorough patient education, and setting realistic expectations. Our multidisciplinary team supports patients from cancer removal through healing and long-term follow-up.
Contact Us
If you or a loved one requires skin cancer reconstruction, our experienced surgeons at the Texas Center for Facial Plastic Surgery are here to help restore confidence and function with personalized care.
Frequently Asked Questions (FAQs) About Skin Cancer Reconstruction
Q: What is Mohs micrographic surgery and why is it used?
A: Mohs surgery is a precise technique to remove skin cancer layer by layer while examining each layer under a microscope. This ensures all cancer cells are removed while sparing as much healthy tissue as possible, reducing recurrence and optimizing reconstruction outcomes.
Q: How soon after skin cancer removal can reconstruction be performed?
A: Reconstruction is often done immediately after cancer removal during the same surgical appointment to promote faster healing and reduce the number of procedures. In some cases, delayed reconstruction may be recommended.
Q: What factors determine the type of reconstruction used?
A: The size, depth, and location of the defect, as well as the surrounding skin’s flexibility and quality, influence the reconstructive technique selected. Patient health and preferences also play a role.
Q: Will I have visible scars after reconstruction?
A: Our surgeons strive to minimize scarring by using specialized techniques and aligning incisions along natural skin lines. While some scarring is inevitable, careful reconstruction often results in inconspicuous scars that fade over time.
Q: Is skin cancer reconstruction painful?
A: Most reconstruction procedures are performed under local or general anesthesia, so patients feel little to no pain during surgery. Postoperative discomfort is managed with medications and typically subsides within days to weeks.
Q: What is the recovery time after reconstruction?
A: Recovery depends on the extent and type of reconstruction. Minor procedures may heal within 1-2 weeks, while complex repairs might require several weeks for swelling and bruising to resolve fully.
Q: Are there risks or complications associated with reconstruction?
A: As with any surgery, risks include infection, bleeding, or healing issues. Our team takes precautions to minimize these risks and monitors patients closely during recovery.
Q: How can I prepare for reconstruction surgery?
A: Follow your surgeon’s instructions, which may include avoiding certain medications, fasting before surgery, and arranging transportation home. Inform your provider about all health conditions and medications.
Q: Will reconstruction affect my facial function?
A: The goal is to restore and preserve facial function, such as blinking, smiling, and breathing. Our surgeons carefully plan reconstruction to maintain or improve these functions.
Q: Can skin cancer recur after reconstruction?
A: While Mohs surgery offers the highest cure rate, close follow-up is important to detect any recurrence early. Prompt treatment can be provided if new skin cancers develop.
Testimonials


