Care Protocols for the Injured Older Adult
Original Date: 06/2023
Purpose: To summarize existing guidelines to optimize care of the injured older adult.
Identification of vulnerable geriatric patients
- Frailty syndrome screening and diagnosis
- Hospitalists using the frailty assessment on their patient intake i.e. H&P.
Problem list – R54 Frailty or Frailty syndrome in geriatric patients - Frailty screening as nursing assessment at time of admission, triggered by location and age (≥ 55) and calculation of frailty score
- Hospitalists using the frailty assessment on their patient intake i.e. H&P.
- Frailty syndrome assessment and management
- Focus on optimization of comorbid medical conditions
- Delirium Prevention Bundle
- Nutrition consult and evaluation
- Depression screen
- Social worker evaluation of social support network
- Physical/Occupational Therapy consult and evaluation
Identification of patients who will benefit from the input of a health provider with geriatric expertise
- Geriatric trauma patients (age ≥ 65) are identified and admitted to the Geriatric Trauma Service (GTS) per established guidelines (https://med.uth.edu/surgery/geriatric-trauma-service).
- Patients are evaluated by the trauma service prior to GTS admission if they meet established trauma consult criteria (https://med.uth.edu/surgery/trauma-team-consultation-policy).
Prevention, identification, and management of dementia, depression, and delirium
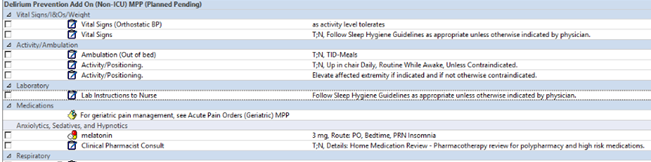
- Delirium prevention bundle MPP

- Nursing education in summer and fall CAVE – B-CAM, sleep hygiene, pain management strategies discussed. This is ongoing and recurrent.
- Geriatric friendly clocks, activity kits used on the floors
- Trauma and Depression Screening (PTSD5) completed by nursing on admission, weekly, and time of discharge
Process to capture and document what matters to patients, including preferences and goals of care, code status, advanced directives, and identification of a proxy decision maker
- Social worker template addresses MPOA, and presence of advance directives
- For DNR patients, advance care planning note would have details as well.
- SITU IHI certified for what matters most 4 M’s (What Matters, Mentation, Medication and Mobility)
Medication reconciliation and avoidance of inappropriate medications
- Delirium Prevention Bundle MPP
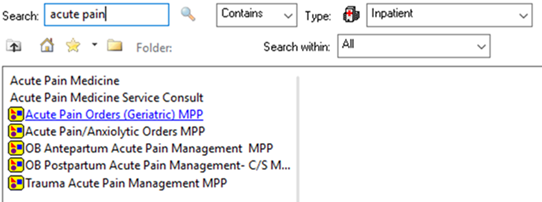
- Geriatric Multimodal pain management MPP
- Medicine reconciliation form and clinical pharmacist review of medications
- Minimization of nighttime awakening for medication administration (VTE prophylaxis guideline revision)
- Select sleep hygiene guidelines to minimize nighttime awakening for vital signs and labs
Screening for mobility limitations and assurance of early, frequent, and safe mobility
- Criteria for PT/OT assessment. (https://med.uth.edu/surgery/trauma-service-pt-ot-consultation/)
Implementation of safe transitions to home or other healthcare facility
- Social worker and case manager evaluation with physician input