Our Research Projects 2
Allergy & Immunology Research

SDOH and Health Disparities in Airway Diseases
Our research on social determinants of health and health disparities focuses on identifying gaps and the factors that contribute to these disparities among patients with airway disease as a means of potentially highlighting targets for improving access and treatment to close the gaps.
 Our chronic rhinosinusitis (CRS) studies target the multidirectional challenges behind the complicating factors driving disease causation, development, and consequence. We explore the role of the nasal and gut microbiome, sleep, cognition, racial and socioeconomic disparities, and immune control in influencing CRS severity and comorbidities. Through the integration of clinical data, multi-omics profiling, and neurocognitive assessments, our goal is to identify biological mechanisms, increase diagnostic precision, and develop tailored treatment plans to enhance patient outcomes.
Our chronic rhinosinusitis (CRS) studies target the multidirectional challenges behind the complicating factors driving disease causation, development, and consequence. We explore the role of the nasal and gut microbiome, sleep, cognition, racial and socioeconomic disparities, and immune control in influencing CRS severity and comorbidities. Through the integration of clinical data, multi-omics profiling, and neurocognitive assessments, our goal is to identify biological mechanisms, increase diagnostic precision, and develop tailored treatment plans to enhance patient outcomes.
Related Projects:
Cognitive Function in CRS
 This study aims to understand and describe the problems associated with memory, language, thinking, or judgment in patients with chronic sinus disease, a condition with long lasting symptoms of nasal congestion and inflammation in the sinuses.
This study aims to understand and describe the problems associated with memory, language, thinking, or judgment in patients with chronic sinus disease, a condition with long lasting symptoms of nasal congestion and inflammation in the sinuses.
With a goal to characterize cognitive function profile in both healthy controls and patients with chronic inflammation in upper airways; and identify those at risk of impaired cognition; as well as identify the preventable risk factors of cognitive impairment including sleep timing shift; and to test the hypothesis that serum IL-6 has a role in this process and may serve as a biomarker for cognitive impairment in CRS.
CRS & Sleep
 With support from the NIH R03 grant and additional private funding, our studies are revealing the strong link between chronic rhinosinusitis (CRS), sleep problems, and treatment outcomes. We found that over half of CRS patients experience sleep apnea and poor sleep quality, emphasizing the need for improved screening and management. Using objective sleep assessments, we confirmed that CRS-related sleep issues are common and often underestimated. Our results also show that inflammation, especially elevated IL-6 levels, plays a key role in these disruptions and impacts treatment response. We also discovered that therapies like exhalation-delivered nasal steroids significantly enhance both sleep quality and sinonasal symptoms, with the biggest benefits observed in patients with lower IL-6 levels and no asthma. We are continuing our research to better understand how CRS, sleep apnea, inflammation, and targeted treatments interact, aiming to develop personalized strategies to improve sleep and overall quality of life for people living with CRS.
With support from the NIH R03 grant and additional private funding, our studies are revealing the strong link between chronic rhinosinusitis (CRS), sleep problems, and treatment outcomes. We found that over half of CRS patients experience sleep apnea and poor sleep quality, emphasizing the need for improved screening and management. Using objective sleep assessments, we confirmed that CRS-related sleep issues are common and often underestimated. Our results also show that inflammation, especially elevated IL-6 levels, plays a key role in these disruptions and impacts treatment response. We also discovered that therapies like exhalation-delivered nasal steroids significantly enhance both sleep quality and sinonasal symptoms, with the biggest benefits observed in patients with lower IL-6 levels and no asthma. We are continuing our research to better understand how CRS, sleep apnea, inflammation, and targeted treatments interact, aiming to develop personalized strategies to improve sleep and overall quality of life for people living with CRS.
CRS & Nasal Microbiome
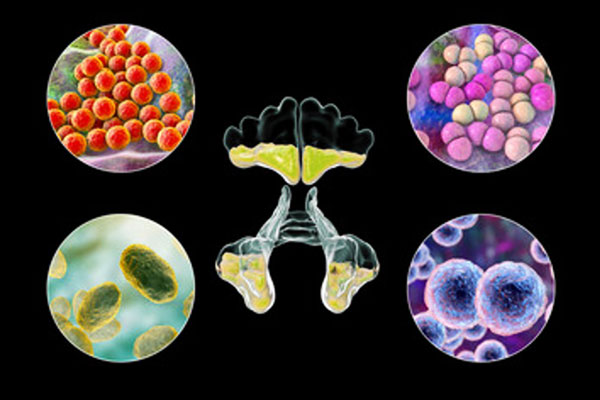 There is growing evidence that the nasal microbiome plays a major role in the development and course of CRS. Microbial diversity and composition have been linked to chronic sinonasal inflammation, and it is thus essential to understand how these alterations influence disease. We have shown microbial dysbiosis in CRS to be linked with reduced diversity and with microbial community imbalance, potentially to increase chronic mucosal inflammation as well as to add to greater symptoms. In response, this study measures longitudinal change in the nasal microbiome in subjects with CRS undergoing endoscopic sinus surgery (ESS) versus controls undergoing ESS for pituitary tumor resection to isolate surgery-related effects from disease-related alterations. This research aims to gain a deeper understanding of how therapeutic interventions, such as surgery, topical steroid irrigations, and proton pump inhibitors (PPIs), affect the nasal microbial ecosystem over the long term. Aids to the development of targeted microbiome-directed methods for the improvement of CRS management and patient outcomes can be gleaned from these findings.
There is growing evidence that the nasal microbiome plays a major role in the development and course of CRS. Microbial diversity and composition have been linked to chronic sinonasal inflammation, and it is thus essential to understand how these alterations influence disease. We have shown microbial dysbiosis in CRS to be linked with reduced diversity and with microbial community imbalance, potentially to increase chronic mucosal inflammation as well as to add to greater symptoms. In response, this study measures longitudinal change in the nasal microbiome in subjects with CRS undergoing endoscopic sinus surgery (ESS) versus controls undergoing ESS for pituitary tumor resection to isolate surgery-related effects from disease-related alterations. This research aims to gain a deeper understanding of how therapeutic interventions, such as surgery, topical steroid irrigations, and proton pump inhibitors (PPIs), affect the nasal microbial ecosystem over the long term. Aids to the development of targeted microbiome-directed methods for the improvement of CRS management and patient outcomes can be gleaned from these findings.

Impact of Circadian-Microbiome Interaction on the Gut-Pancreas Axis in Aging
This research aims to understand the modality and contributing factors of healthy aging. In this study, we aim to examine the role of abnormal eating time (a common lifestyle factor that affects circadian rhythm) in accelerating aging by modulating intestinal barrier damage, microbiota dysbiosis, gut leakiness, and pancreatic damage.
Microbial signaling networks and their interaction with host biological rhythms as targetable mechanisms involved in aging will be studied. Findings from these experiments will identify intervenable mechanisms to prevent organ damage by age.
Two enrollment sites:
UTHealth Houston
- PI: Faraz Bishehsari, MD, PhD
- Co-investigator: Mahboobeh ‘Maha’ Mahdavinia, MD, PhD
Brownsville
- Co-investigators:
Pediatrics Allergy & Immunology Research
 The PERSIAN birth cohort is a project that focuses on understanding how genetics, socioeconomic, environmental, and psychological factors contribute to health and disease in the Iranian population.
The PERSIAN birth cohort is a project that focuses on understanding how genetics, socioeconomic, environmental, and psychological factors contribute to health and disease in the Iranian population.
In this collaboration, our research has primarily focused on the incidence of food allergy and atopic comorbidities in children from birth to early childhood. We also compare the stool microbiome between children in South Africa and Iran to better understand the prevalence of IgE-mediated food allergy.

Food Allergy Outcomes Related to White and African American Racial Differences (FORWARD)
We are part of the FORWARD study, a prospective, multi-site NIH-funded research project focused on pediatric food allergies and atopic diseases. With over 1,500 children enrolled across four partner sites in the U.S., this study examines the natural history of food allergies and related comorbidities, including asthma, eczema, and other atopic conditions. Our research explores multiple contributing factors, including the impact of the gut and skin microbiomes on allergy onset, persistence, and resolution patterns. The study also examines racial and ethnic disparities to better understand how these factors influence allergy development and outcomes, aiming to improve care for children across diverse populations.

PCD & Transcriptomics
Previous Projects:

This study aims to determine the prevalence of IgE-mediated food allergy in unselected South African children aged 12-36 months in an urban region in the Western Cape and a rural cohort of Xhosa children in the Eastern Cape, and to describe the prevalence of various modifiable and non-modifiable risk factors.
View Dr. Mahboobeh Mahdavinia’s full list of publications »