Improving Survivorship in Head and Neck Cancer: UTHealth Department of Otorhinolaryngology and Institute of Molecular Medicine Partner on CPRIT Research Award
 A $605,425 grant from the Cancer Prevention Research Institute of Texas (CPRIT) will enable researchers at The University of Texas Health Science Center at Houston (UTHealth) to adapt night-goggle technology used by the military to visualize the workings of the lymphatic system in head and neck cancer patients. The grant was awarded to principal investigator Eva Sevick, PhD, professor of molecular medicine and Kinder Chair at UTHealth’s Institute of Molecular Medicine (IMM). At the IMM, Dr. Sevick leads one of four National Cancer Institute Centers for Translational Research, which focuses on new imaging instrumentation, algorithms and imaging agents and their clinical translation. Ron Karni, MD, assistant professor in the department of Otorhinolaryngology-Head and Neck Surgery, and I-Chih Tan, PhD, research engineer at the IMM, are co-investigators for the clinical trial.
A $605,425 grant from the Cancer Prevention Research Institute of Texas (CPRIT) will enable researchers at The University of Texas Health Science Center at Houston (UTHealth) to adapt night-goggle technology used by the military to visualize the workings of the lymphatic system in head and neck cancer patients. The grant was awarded to principal investigator Eva Sevick, PhD, professor of molecular medicine and Kinder Chair at UTHealth’s Institute of Molecular Medicine (IMM). At the IMM, Dr. Sevick leads one of four National Cancer Institute Centers for Translational Research, which focuses on new imaging instrumentation, algorithms and imaging agents and their clinical translation. Ron Karni, MD, assistant professor in the department of Otorhinolaryngology-Head and Neck Surgery, and I-Chih Tan, PhD, research engineer at the IMM, are co-investigators for the clinical trial.
“Adapting infrared night-goggle technology in a new way is allowing us to visualize things we’ve never before seen in either animals or human beings,” Dr. Sevick says. “We thought, ‘Eureka! We’re actually seeing the workings of the lymphatic system in living beings.’ Based on what we discover in the clinical trial, we’re hoping to be able to cure head and neck cancer in a more efficient way that improves the overall quality of life of patients.”
Following treatment for their disease, 50 percent of head and neck cancer patients suffer profound lymphedema, swelling due to blockage of the lymph vessels that drain fluid from tissues throughout the body and allow immune cells to travel where they are needed. “During treatment for head and neck cancer, the lymphatic system receives three types of injuries,” says Dr. Karni, who specializes in transoral robotic surgery (TORS) for the treatment of head and neck cancer. “The first is caused by the tumor itself, which infiltrates the lymph system and impedes circulation. Surgery to remove all the lymph nodes in the neck is an assault on the body. The third injury is radiation. Almost all patients with advanced head and neck cancer receive radiation therapy, which seals the lymphatics. Patients undergoing treatment for head and neck cancer usually have fibrosis, very limited movement of the head and neck and lymphedema, which causes debilitation and deformity. We don’t know exactly why the lymph vessels stop pumping, and we hope to gain new information during the course of the study.”
Dr. Sevick has pioneered the development of near-infrared (NIR) fluorescence optical imaging and tomography for molecular imaging. Her research team is active in preclinical small animal imaging with nuclear and optical techniques and is pioneering diagnostic imaging for nodal staging in cancer. For the CPRIT-funded study, she and Dr. Tan took night-goggle technology and developed it into a detector – a very small device that uses a charge-coupled device (CCD) chip similar to the chip in a digital camera.
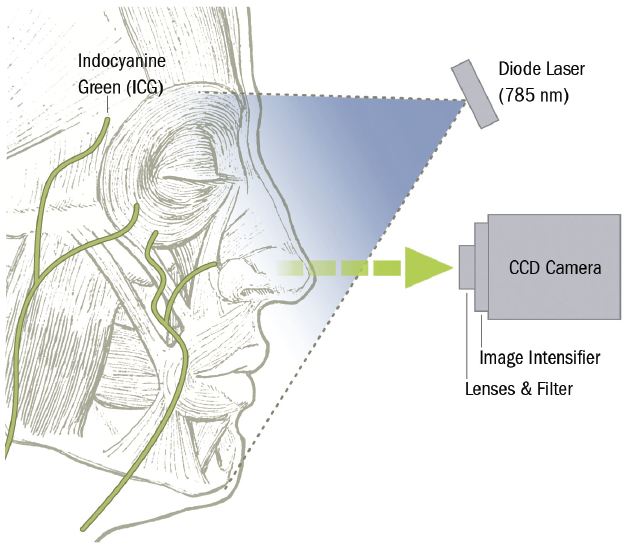
Dr. Sevick has pioneered the development of NIR fluorescence optical imaging and tomography for molecular imaging. Her team took night-goggle technology and developed it into a detector—a very small device that uses a CCD chip similar to that used in a digital camera.
They have also been developing new dyes that fluoresce. “Near-infrared light propagates through several centimeters of tissue,” she says. “It’s non-ionizing with no exposure to radioactivity. If we inject a tiny bit of fluorescent dye, it’s taken up by the lymphatic system, allowing us to see the lymph vessel segments that pulse in real time as they pump lymph through the body as little ‘lymph hearts.’”
Dr. Sevick and Dr. Karni note that head and neck cancer survivorship issues have been overlooked until recently. “As we become more efficient at curing cancer, we have to start looking at the aftermath of treatment,” Dr. Sevick says. “Our patients are cured, but living with lymphedema is very expensive, and often they don’t know where to go for help.”
The Memorial Hermann Wound Care Center at Memorial Hermann-Texas Medical Center, under the direction of hyperbaric medicine specialist Erik Maus, MD, operates a Lymphedema Management Center to treat patients with chronic and acute non-healing wounds. The Center also has a clinical research program that provides state-of-the-art options for wound management.
“The clinical trial is an incredible opportunity for us to impact the lives of our cancer survivors,” Dr. Karni says. “In many cases the cure we provide causes new disease. Cancer survivorship research – looking beyond the cure to what happens afterwards – is a relatively new and exciting area of focus. Through this feasibility study we want to visualize how lymphatics work during metastasis, treatment and recovery to develop an understanding of how lymphatics respond to the cancer itself and the treatment.”
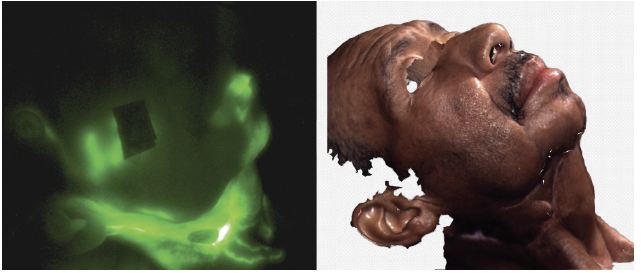
Near-infrared light propagates through several centimeters of tissue. When fluorescent dye is injected, researchers can see the lymph vessel segments pulse in real time as they pump lymph through the body.
The researchers are currently recruiting patients, who will be imaged in Dr. Karni’s office using the technology developed in Dr. Sevick’s lab. A near-infrared fluorescence snapshot will be taken before the start of treatment, after surgery, after radiation therapy and for a year following treatment of each subject.
“We’d like to discover why half of patients treated for head and neck cancer get lymphedema and others don’t,” Dr. Sevick says. “This study has implications for other types of cancer as well. It’s an incredible opportunity for us to impact the lives of our cancer survivors. The incidence of head and neck cancer is increasing because of human papillomavirus. We’re seeing younger and younger people with the disease, and lost productivity due to disease has a significant economic impact. We’re working to mitigate survivorship disease.”
The NIR fluorescence imaging system is located in Dr. Karni’s office. “We expect to get a treasure trove of data about how lymphatic pathways reorient around the surgical and radiation site,” he says.
“If this works as well as we think it will, we’ll be better able to stage head and neck cancer,” Dr. Sevick says. “If we can ultimately identify the lymph nodes that are cancer positive, remove them and leave the others, we may become more efficient at treatment and reduce the risk of lymphedema.”
To refer a patient to the clinical trial, call Karen Gore at 713-500-3435 or Dr. Karni at 713-486-5000.