Colorectal Conditions & Treatments
Colorectal Cancer is the 2nd Leading Cause of Cancer-Related Deaths Among Adults in the US
A Colonoscopy Screening Can Help Save Your Life
Colon cancer doesn’t always show signs. That’s why it’s important to schedule a screening regularly. According to the American Cancer Society, colonoscopy screenings and polyp removal help prevent colon cancer and decrease the number of colorectal cancer deaths.
If you have no family history of colorectal disease, you should have a colonoscopy by age 45. If you do have a family history, the age to get screened is ten years before your family member’s colorectal disease first occurred. For example, if a family member was diagnosed at 35 years old, you should schedule a colonoscopy at 25 years old.
Colonoscopies are a safe, effective way to examine the full lining of the colon and rectum, diagnose colorectal problems, and ensure your health. At UT Physicians Colon and Rectal Clinic, our colorectal specialists perform over 8,000 procedures yearly.
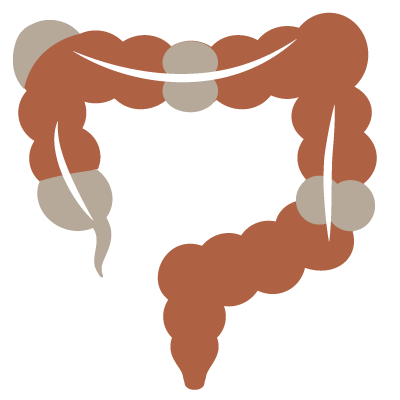
What is Colorectal Cancer
The term colorectal cancer is used to describe both colon and rectal cancers. As the area’s leading experts in treating colorectal diseases and disorders, Our Colon and Rectal Surgeons provide the most advanced medical options available for the prevention and treatment of both.
Who is at Risk?
Colorectal cancer affects men and women equally, and the risk increases after age 50. Additional risk factors include having a chronic inflammatory bowel disease such as ulcerative colitis or Crohn’s disease or having a parent, sibling, or child with colorectal cancer or polyps.
Prevention
Colorectal cancer is preventable and treatable. Colorectal cancer is treatable and potentially curable when detected in its initial stages. The American Society of Colon and Rectal Surgeons reports that 80-90% of patients are restored to normal health if the cancer is diagnosed and treated early.
Prevention starts with a screening colonoscopy. Almost all colorectal cancers begin as benign polyps in the colon. We can quickly find and remove polyps during a screening colonoscopy, preventing them from becoming cancer. UT Physicians Colon and Rectal Clinic recommends you have a screening colonoscopy at age 45 and as advised by your physician after that.
Healthy choices help prevent colorectal cancer. While screening colonoscopies can prevent colorectal cancer by detecting polyps, a healthy lifestyle also goes a long way toward circumventing the disease. There are many simple choices you can make to help keep colorectal cancer at bay:
- Exercise
- Maintain a healthy weight
- Eat high-fiber foods
- Avoid high-fat foods
- Don’t smoke
Colorectal Cancer Symptoms
Often, early colorectal cancer has no symptoms at all. This is why a screening colonoscopy is vitally important. Other times, the first sign of colorectal cancer is a low red blood cell count (anemia) due to undetected internal bleeding.
But many times, there are clear warning signs. Colorectal cancer may cause one or more of the following symptoms:
- A change in bowel habits (e.g., diarrhea, constipation, narrowing of the stool, etc.) lasting more than a few days
- A feeling that you need to have a bowel movement that is not relieved by doing so
- Rectal bleeding
- Blood in the stool, which may cause the stool to look dark
- Cramping or abdominal pain
- Weakness and fatigue
- Unintended weight loss
Other non-cancerous conditions such as infection, hemorrhoids, irritable bowel syndrome, and inflammatory bowel disease may also exhibit similar symptoms. If you experience one or more, see your doctor immediately to find and treat the cause.
Colorectal Cancer Treatment Options
Despite its high recovery rate, colorectal cancer remains the second-most common cause of cancer deaths in the United States. Prevention is best. But if you are among the 140,000 people affected by the disease each year, UT Physicians Colon and Rectal Surgery can help.
Robotic colorectal surgery begins much like traditional laparoscopic surgery. Once the patient is anesthetized, one of our certified robotic colorectal surgery specialists makes four tiny incisions, inserts trocars, and inflates the abdominal cavity. The surgeon then docks the robotic unit—a four-armed device that operates a laparoscope and up to three specialized surgical instruments—into the trocars and moves to a separate console. Using a high-definition 3-D monitor and hand controls, your surgeon can perform the operation with unprecedented precision and is always in complete control—the robot cannot move without instructions from the surgeon.
Laparoscopic colorectal surgery is a minimally invasive surgical technique in which a micro-camera and micro-instruments are used to view the contents of the abdomen and perform surgery. UT Physicians are renowned experts in laparoscopic colorectal surgery and frequently lead national teaching seminars on the subject. Our specialists perform most of all colorectal surgeries laparoscopically, thus assuring patients faster recovery and less pain than traditional invasive methods used by 80% of surgeons.
Transanal endoscopic microsurgery (TEMS) is a minimally invasive outpatient procedure used to remove rectal polyps or growths that are too high or too large to access via colonoscopy or traditional invasive transanal methods, thus avoiding abdominal surgery. Performed through the anus, no incisions are needed, and patients typically feel no pain during the procedure. TEMS is used specifically to treat early rectal cancers and has a much lower rate of polyps recurrence compared to standard transanal removal.
Transanal minimally invasive surgery (TAMIS) is a newer minimally invasive technique for performing local excision of well-selected rectal neoplasms. It utilizes a single-incision laparoscopic port as access into the rectal vault. TAMIS provides a quality of surgical resection similar to TEM.
Bowel or fecal incontinence is the inability to control a stool until a socially acceptable time. This condition ranges in degree of severity and affects approximately 7% of the population. It is more common in women and occurs in a wide age range. There are a variety of treatments for fecal incontinence. Unfortunately, due to embarrassment or lack of information, many people fail to seek help. UT Physicians Colon and Rectal Surgeons have a special interest in fecal incontinence and strives to provide our patients with the latest treatment options. One of the advanced procedures offered for more severe cases is the use of Interstim® Therapy (also known as Sacral Nerve Stimulation).
In Office Diagnostic Options
Pelvic Floor Testing (Anal Manometry) – Since there are many causes of fecal incontinence, it is essential to determine the cause and severity through careful history taking, physical examination, and specialized testing called pelvic floor testing, which may include anal manometry, rectal sensation, pudendal nerve testing, and anal ultrasound. UT Physicians Colon and Rectal Clinic Physicians utilize this group of minimally invasive tests to help determine sensation in the anal canal or rectum, measure the pressures of the anal sphincter muscles, and test for nerve damage.
Fecal Incontinence Non-Surgical Treatments
Bowel Evacuation Programs – Education on lifestyle changes that may help lessen bowel accidents include fiber supplements, suppositories, nutrition recommendations, and antidiarrheal medications if indicated.
Physical Therapy and Biofeedback – Non-invasive management of fecal incontinence can include biofeedback therapy and pelvic floor retraining with specialized pelvic floor physical therapists to help strengthen the anal sphincter muscles and improve bowel control.
Fecal Incontinence Surgical Treatments
Sacral Neuromodulation (InterStim® and Axonics®) – This is one of the most leading-edge technologies available for the treatment of fecal incontinence. Originally developed for treating urinary incontinence and frequency, Sacral Neuromodulation has also been proven to significantly help those suffering from bowel incontinence by gently stimulating the nerves that control the bowel to help restore more normal control. The procedure is done as an outpatient procedure in two phases.
The first phase allows the patient to test the therapy for 1-2 weeks. If significant improvement is documented, the second phase for long-term therapy is scheduled.
The Evaluation Phase: To determine if sacral neuromodulation will be an effective therapy, a short testing period is required in which a small wire is placed under the skin near the tailbone during an outpatient procedure. This wire is connected to an external trial stimulator (worn temporarily near the lower back or hip) and sends mild electrical pulses to the nerves that help control bowel function. Patients are asked to document daily symptoms on a bowel diary to determine if enough improvement is experienced to move forward with the long-term device.
 Long-Term Therapy: If the patient and the physician determine that enough improvement was successfully observed and documented during the evaluation phase, they are candidates for long-term therapy. During the second outpatient procedure, a small implantable device (“pacemaker”) will be placed just beneath the skin in the upper part of the buttock. The device will send mild stimulation to the pelvic nerves that assist in the communication between the brain and the muscles and nerves that control bowel function. The stimulation can be controlled and adjusted with the use of a small patient remote control.
Long-Term Therapy: If the patient and the physician determine that enough improvement was successfully observed and documented during the evaluation phase, they are candidates for long-term therapy. During the second outpatient procedure, a small implantable device (“pacemaker”) will be placed just beneath the skin in the upper part of the buttock. The device will send mild stimulation to the pelvic nerves that assist in the communication between the brain and the muscles and nerves that control bowel function. The stimulation can be controlled and adjusted with the use of a small patient remote control.
Sphincteroplasty – A majority of patients with fecal incontinence have a separation of their anal sphincter muscle due to prior child birthing or prior surgery. These patients are candidates for an anal sphincter repair. Typically, patients are in the hospital for several days after surgery, with a post-operatively recovery period of 2-4 weeks. Good outcomes with fewer bowel accidents are obtained in this select patient population.
What is an Anal Abscess?
An anal abscess is an infected cavity filled with pus located near the opening of the anal canal. Symptoms of an anal abscess include constant pain and swelling. Other possible symptoms include fever, feeling poorly, and drainage of pus. By draining the pus from the infected cavity with an incision, your UT Physicians Colon and Rectal Surgeon can effectively treat this abscess. Often, we conduct the treatment in our office using a local anesthetic. A large or deep abscess might need to be drained in the operating room. Sometimes a small catheter remains in the incision for several days to ensure adequate drainage. Antibiotics alone are not an alternative to draining the pus.
What is an Anal Fistula?
An anal fistula will form in about 50 percent of all abscess cases. An anal fistula is usually the result of a previous abscess. It is a persistent abnormal passage or tunnel between the interior of the anal canal or rectum and the skin surface where the abscess drains. If the outside opening of the tunnel heals, recurrent abscesses develop. UT Physicians Colon and Rectal Surgeons recommend surgery to cure an anal fistula. While some anal fistulas are simple to treat, others require special attention to limit any damage to the sphincter muscles. A complicated fistula may require repair using a flap of tissue or new products like plasma-rich protein (PRP)/Amniotic fluid.
What is an Anal Fissure?
An anal fissure is a small tear or cuts in the skin lining the anus, which can cause pain and/or bleeding. The pain typically is sharp and is worse with bowel movements. The most common cause is a hard, dry bowel movement. Other causes of an anal fissure include diarrhea and inflammation of the anorectal area. Anal fissures may be acute (recent onset) or chronic (present for a long time or recurring frequently). Spasm of the anal sphincter muscles contributes to the pain and hinders healing. Over 90% of acute anal fissures managed with non-operative treatments will heal without surgery. Chronic fissures may require your Surgeon to perform surgery where a small portion of the sphincter muscle is cut to relieve the spasm and allow healing. In some cases, our team will offer patients Botox injections to aid in recovery.
Four out of five people will experience hemorrhoids in their lifetime. Also known as piles, hemorrhoids are essentially swollen or inflamed veins in the anal canal. Internal hemorrhoids form inside the anal canal, while external hemorrhoids swell near the opening of the anus.
The exact cause of hemorrhoids is unknown, but several factors can contribute to their development, including chronic constipation or diarrhea, pregnancy, aging, straining during bowel movements, overuse of laxatives or enemas, prolonged sitting on the toilet (e.g., reading, etc.) and being overweight. Suitable preventative methods, such as limiting prolonged sitting on the toilet, avoiding the overuse of laxatives and enemas, and keeping a healthy diet rich in fresh vegetables, fruits, and whole grains, are often all you need to prevent or relieve hemorrhoids.
Get Hemorrhoid Relief That Works
If you think you might have hemorrhoids, the first step toward treatment and relief is recognizing the symptoms:
- Rectal bleeding
- Pain
- Protrusion during bowel movements
- Sensitive lump(s)
- Unusual itching
If you’re experiencing these symptoms, let us help you find hemorrhoid relief. A board-certified colorectal specialist at our UT Physicians Colon & Rectal Clinic can evaluate, diagnose and discuss treatment options. Although not usually serious, hemorrhoids can be painful, and other diseases can cause some symptoms, so delay in treatment can be dangerous. Without a proper diagnosis, you may suffer much longer than necessary.
Hemorrhoid Treatment
We offer the most up-to-date innovations in hemorrhoid treatment. After a complete examination to determine the type and severity of your hemorrhoids, our experienced physicians will choose the most effective treatment. Our goal is to get you feeling 100% in no time.
Non-Surgical Options
At UT Physicians Colon and Rectal Clinic, only a small percentage of patients require hemorrhoid surgery. Many mild cases are successfully relieved by diet changes or simple in-office procedures.
Diet & lifestyle changes can often relieve mild hemorrhoid symptoms. These may include increased fluids and fiber (e.g., fruits, vegetables, whole-grain bread and cereals, and fiber supplements), eliminating excessive straining to reduce the pressure on hemorrhoids, and/or sitting in a sitz bath of warm water.
Rubber band ligation works effectively on internal hemorrhoids that bleed or protrude with bowel movements. The procedure involves placing a small rubber band around the hemorrhoid to cut off its blood supply. The hemorrhoid and band fall off in a few days, and the wound usually heals in a week or two.
Transanal hemorrhoidal dearterialization (THD) is a minimally invasive procedure involving a non-excisional ultrasound technique to decrease blood flow to the hemorrhoid(s). Since this procedure does not involve the surgical removal or cutting of the hemorrhoid tissue, it is less traumatic to the body than a hemorrhoidectomy and results in a faster recovery time with minimal discomfort. Patients can usually resume normal activities in 4-5 days. Please visit us to see if you are a candidate for this procedure.
Surgical Options
Occasionally, severe cases may require hemorrhoid surgery performed by a skilled surgeon on an inpatient or outpatient basis.
Hemorrhoidectomy is considered the best surgical method for completely removing external hemorrhoids. Typically performed on an outpatient basis, hemorrhoidectomy is necessary when (1) clots repeatedly form in external hemorrhoids; (2) ligation fails to treat internal hemorrhoids; (3) protruding hemorrhoid cannot be reduced; or (4) there is persistent bleeding. Under anesthesia, a hemorrhoidectomy removes the excess tissue causing the bleeding and protrusion.
Do Hemorrhoids Cause Cancer?
No. There is no relationship between hemorrhoids and cancer. However, the symptoms of hemorrhoids — particularly bleeding, unusual itching, pain, or sensitive lumps around the anal area — are similar to those of colorectal cancer and other digestive system diseases. This is why it is important to have a physician specially trained in treating diseases of the colon and rectum to evaluate your symptoms. Reliance on over-the-counter medicines or other self-treatments is risky at best.
Offering Individualized Care and Treatment
UT Physicians Colon and Rectal Surgery team works closely with you to create a highly individualized treatment plan based on the type and severity of the symptoms. Treatment options may include dietary changes, medications, and, in some cases, surgery. If surgery is necessary, we are experts in laparoscopic procedures to cure or relieve IBD symptoms. The following procedures performed by our team are just three examples of our expertise:
- Laparoscopic Small Bowel Surgery – A small bowel resection is a surgery to remove a diseased section of the small intestine. The laparoscopic technique involves small incisions and faster recovery. In this procedure, the diseased section of the small intestine is stapled and removed; then, the two bowel ends are reattached using staples.
- Laparoscopic J-Pouch Surgery – This procedure can often “cure” those patients with ulcerative colitis as well as eliminate their risk of colorectal cancer. The J-pouch procedure is the common name used for the operation that removes the entire colon and rectum and replaces the rectum with a neorectum, or new rectum, a pouch made from the last portion of the small intestine and connected to the anus.
- Laparoscopic Restorative Proctocolectomy – Restorative proctocolectomy is a standard treatment for advanced IBD. UT Physicians Colon and Rectal Surgeons typically perform this technique via a laparoscopic or minimally invasive approach, while most surgeons often use an open approach, requiring a much larger incision.
Crohn’s Disease Vs. Ulcerative Colitis
Crohn’s disease and ulcerative colitis are so similar they are often mistaken. Both are chronic inflammation in the digestive tract lining, but Crohn’s disease can spread deep into the layers of affected tissues. In contrast, ulcerative colitis usually affects only the innermost lining of the colon and rectum.
Understanding Crohn’s Disease
Crohn’s disease may affect the GI tract anywhere from the mouth to the anus. However, the ileocecal region, the last part of the small bowel with the first part of the colon, is most commonly affected. Treated primarily with medicine, surgery is typically needed at some point during Crohn’s disease. A severe flare of Crohn’s may require hospitalization and emergency surgery. Crohn’s disease in the colon carries an increased risk for colon cancer.
Understanding Ulcerative Colitis
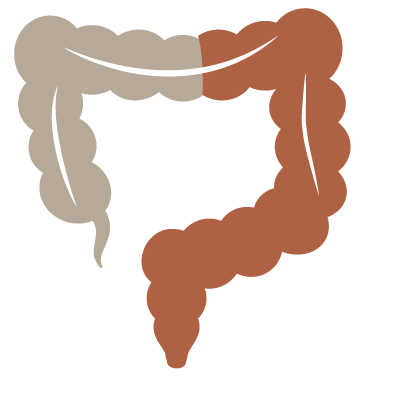 Ulcerative colitis involves the rectum and some or all of the colon. A severe flare of ulcerative colitis may require hospitalization, and if the disease cannot be controlled medically, surgery is necessary. Ulcerative colitis is curable with surgery by removing the entire colon and rectum. In most cases, a permanent ileostomy can be prevented by constructing a pouch made out of small bowel and connected to the anus, called a J-Pouch. Ulcerative colitis does carry an increased risk of colon cancer. Sometimes surgery is recommended based on the duration of the disease or abnormal changes in the colon’s lining called dysplasia that make the risk of colon cancer too high to continue to follow the patient’s medical treatment.
Ulcerative colitis involves the rectum and some or all of the colon. A severe flare of ulcerative colitis may require hospitalization, and if the disease cannot be controlled medically, surgery is necessary. Ulcerative colitis is curable with surgery by removing the entire colon and rectum. In most cases, a permanent ileostomy can be prevented by constructing a pouch made out of small bowel and connected to the anus, called a J-Pouch. Ulcerative colitis does carry an increased risk of colon cancer. Sometimes surgery is recommended based on the duration of the disease or abnormal changes in the colon’s lining called dysplasia that make the risk of colon cancer too high to continue to follow the patient’s medical treatment.
Let our Team Diagnose Your Issue
Symptoms that Crohn’s disease and ulcerative colitis may share include abdominal pain, fever, bleeding, and diarrhea. With Crohn’s disease, some people develop inflammation in their anal region, which may be mistaken for other diseases. Laboratory tests, endoscopic procedures, and radiology tests are used to diagnose IBD. Your colorectal specialist can help you determine the best course of action for diagnosis and treatment.
Crohn’s and Colitis Foundation of America (CCFA)
UT Physicians Colon and Rectal and Gastroenterology Team continues to partner with the CCFA to raise money and increase awareness of IBD-related diseases. The first step to creating more awareness is community involvement. Please help us “take steps” toward a cure and get involved. Visit CCFA.org for more information on upcoming events.
What is an Ostomy?
An ostomy is a surgical procedure that creates an opening for the diversion of waste from the bowel or the bladder. Ostomies are necessary when part or all of the intestine or bladder are removed and may be temporary or permanent. Some conditions that may lead to ostomy surgery include cancer, diverticulitis, polyps, congenital disabilities, ulcerative colitis, Crohn’s Disease, and trauma.
What is a Stoma?
A stoma is an artificial opening created by attaching a portion of your bowel to the skin on your abdomen, allowing waste to be transferred to the outside of the body into a bag or pouch. Depending on the procedure, a stoma can be permanent or temporary, but all stomas require special care.
Adjusting to a stoma can be a significant change, requiring not only medical support but emotional support as well. It’s the goal of UT Physicians Colon and Rectal Clinic to ensure that our patients resume everyday life habits, be independent with their stoma care, and have a positive self-image. Our nurses are trained to help patients modify their stoma care and address their comfort, security, and reliability needs.
Understanding the Various Types of Ostomy
 There are several different types of ostomy:
There are several different types of ostomy:
Colostomy – A surgically created opening in the abdominal wall that allows the passage of digested food. It may be temporary or permanent, depending upon the portion of the colon involved.
 Ileostomy – A small surgically created opening in the small intestine through which digested food passes. It may be temporary or permanent and may involve the removal of all or part of the colon.
Ileostomy – A small surgically created opening in the small intestine through which digested food passes. It may be temporary or permanent and may involve the removal of all or part of the colon.
To learn more about these significant colon and rectal conditions click below and open a new window on the American Society of Colon and Rectal Surgeons website:
- Anal Cancer
- Anal Warts
- Constipation
- Diverticular Disease
- Irritable Bowel Syndrome
- Pelvic Floor Dysfunction
- Pilonidal Disease
- Polyps of the Colon and Rectum
- Pruritus Ani
- Rectocele
UT Physicians Colon and Rectal Clinic, our physicians work with patients at our Pelvic Floor Center to improve pelvic health issues with the latest in pelvic floor therapy. We offer an individualized, multi-disciplinary approach to overcoming the various symptoms of pelvic floor disorders. Our pelvic floor therapy provides innovative solutions to the following:
- Accidental bowel leakage
- Chronic constipation
- Pelvic organ prolapse
- Rectal cancer
Understanding the Pelvic Floor
The pelvic floor consists of muscles, nerves, and connective tissue that support the structures of the pelvis: the rectum, bladder, and female reproductive organs. Over time or with an acute injury, these supportive tissues can weaken, causing incontinence of urine and/or feces and vaginal prolapse, a condition in which the pelvic organs can “fall” into the vagina, causing the tissue to protrude.
Comprehensive Diagnostic Testing
- Anal Manometry – Measures the strength of the internal and external sphincters and coordination of the pelvic floor muscles and assesses sensations in the rectum. Used to determine constipation, and fecal incontinence, to rule out Hirschsprung’s and many other pelvic floor conditions.
- EMG recruitment – Assess the patient’s ability to contract and relax the pelvic floor muscles voluntarily. Used to assess relaxation of the pelvic floor in constipation. Pudendal nerve EMG – Assesses conduction of the pudendal nerve. Mainly used in diagnosing the cause of accidental bowel leakage but also rectal prolapse and enterocele.
- Anal ultrasound – Images sphincters and tissues surrounding the anal canal. Used to assess accidental bowel leakage, fistula, abscess, sphincter injury (post-delivery/surgery), and pain. This in-office procedure involves placing an ultrasound probe in the anorectal canal. While this may cause slight discomfort, it is largely pain-free and provides our surgeons with an excellent understanding of the anatomy of each patient’s pelvic floor.
- Cine Defecography – A test using fluoroscopy that evaluates rectal emptying and relaxation of the pelvic floor. Visualizes rectocele, enterocele, and rectal prolapse.
- PNE (Peripheral Nerve Evaluation) – Determines whether sacral nerve stimulation for the control of accidental bowel leakage or lower urinary tract dysfunction is appropriate for a given patient. A temporary device is used, and, if successful, surgery to implant a permanent device would be the next option.