Research reveals new approach to measure ophthalmic artery blood flow
McGovern Medical School research detailing a novel non-invasive measurement of blood flow in the ophthalmic artery recently was published in Cell Reports Method.
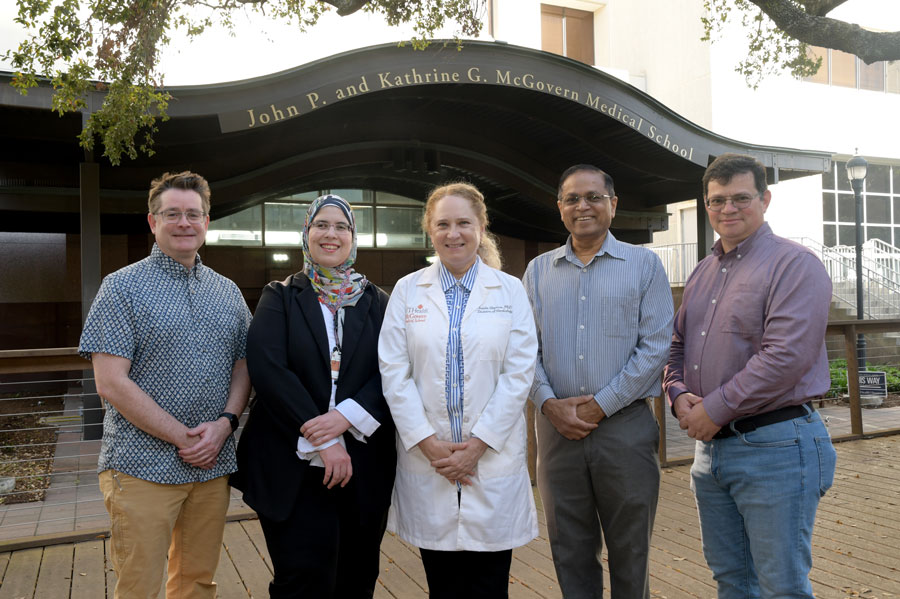
Led by Iraida Sharina, PhD, associate professor of Internal Medicine, Cardiology, the paper, “Non-invasive Real-time Pulsed Doppler Assessment of Blood Flow in Mouse Ophthalmic Artery,” was published in the Feb. 24 issue. The research was completed in collaboration with Anilkumar Reddy,PhD, from Baylor College of Medicine, and Sean Marrelli, PhD, professor, Department of Neurology.
The ophthalmic artery (OphA) is essential for the health of the eye and compromised OphA blood flow is a critical contributor to various eye pathologies. Presently, there is a lack of direct non-invasive methods to measure OphA blood flow, Sharina explained.
This research presents a new application of pulsed-Doppler ultrasound to provide real-time, non-invasive measurement of blood flow velocity in OphA through an identified soft tissue window in the mouse head, which allows assessing a blood flow signal from OphA without surgically opening the skull.
“The method we present here allows for non-invasive assessment of blood flow parameters in OphA at its point of emergence from within the cranium and into the orbit,” she explained. “This approach enables longitudinal experiments in the same animal and eliminates the need for invasive procedures to assess OphA in mice. The high time-resolution, accuracy, and reproducibility of the presented approach combined with reduced data variability enables characterization of the kinetics of drug responses with previously unmatched temporal resolution.”
This convenient method can be used for the specific evaluation of the OphA function, drug screenings or as a surrogate approach to study vascular pathology of cerebral arteries deriving from the internal carotid artery in mice, she added.
Sharina said the idea to publish this technical manuscript came from the realization that numerous other small research groups need a convenient approach to test and validate ideas on cerebrovascular function without a major investment of time and funds. “Our method allows us to bypass two major problems in staging of the experiment: time and labor consuming surgical intervention and acquisition of expensive equipment. Equally important, it allows longitudinal and repetitive experiments on the same animal when needed,” she said.
The newly described method will provide a simple and low-cost approach for screening drugs targeting ophthalmic blood flow and may be used beyond the eye. “Important similarities with cerebral vasculature and internal carotid artery origin of OphA make it convenient to use as a surrogate for studies of cerebrovascular pathological mechanisms in various disease states,” she added. “I believe that our method will advance the toolset needed for basic research to investigate and combat ophthalmic and cerebrovascular pathologies.”
Sharina stressed the collaborative nature of the research. “We are deeply thankful to Dr. Anilkumar K. Reddy’s for his original idea to apply pulsed Doppler ultrasound for non-invasive measurement of arterial blood flow in orbital opening of the mouse. His research group graciously provided the Doppler flow velocity measurement system, previously developed to characterize vascular physiology in mice. His help and guidance with mouse surgeries was indispensable for conducting the experiments.
“Dr. Sean P. Marrelli played a vital role in confirming the identity of the targeted artery and mapping its origin from the internal carotid artery by applying microcomputed tomograph vascular imaging, Dr. Emil Martin provided his expertise in pharmacology of vasodilative compounds and helped with the design of experiments with pharmacological challenge of OphA blood flow, and Dr. Radwa Awad, an echo-cardiologist from Egypt with a deep interest in scientific research, and Soren Cobb, summer research medical student in my laboratory, played critical roles in performing a majority of the experiments and analyzing the collected data.”
Cobb was a member of the Summer Research Program in 2022 and won second place in the C. Frank Webber Prize for Student Research.