Initial CENTURY Trial results published in European Heart Journal
A culmination of 15 years of research led by K. Lance Gould, MD, professor of cardiology, The Martin Bucksbaum Distinguished University Chair, and executive director of the UTHealth Houston Weatherhead PET Imaging Center, has resulted in the publication of the first major conclusions of the long-term, randomized CENTURY Trial in the European Heart Journal.
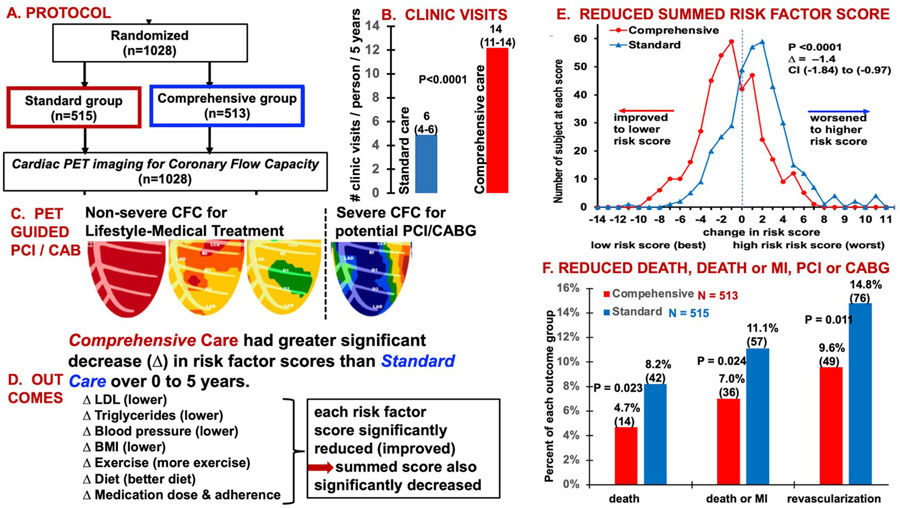
The randomized CENTURY trial tested the hypothesis that a comprehensive strategy integrating intense lifestyle modification and aggressive medical management to goals with revascularization reserved for severely reduced coronary flow capacity (CFC) by positron emission tomography (PET) would reduce risk factors, subsequent revascularization, death and myocardial infarction (MI) compared with standard of care in chronic stable coronary artery disease (CAD).
Between 2009–2017, 515 patients were assigned to comprehensive care and 513 to standard care and followed for 5 or more years. Comprehensive versus standard care decreased risk factors, demonstrating that comprehensive integrated lifestyle modification and medical management toward goals with revascularization reserved for severely reduced CFC, significantly reduced risk factor scores, death, death or MI, and revascularization.
Patients with symptoms, high-risk factors, or even known coronary artery disease commonly present to a physician who orders blood tests, cardiac ultrasound, and a stress test with or without standard nuclear imaging. The cumulative results may be normal, equivocal, mildly or distinctly abnormal, and referred to a cardiologist who may do a coronary angiogram as the “diagnostic gold standard,” to be sure of not missing significant CAD. Any visually “significant” coronary stenosis is then stented or goes to bypass surgery.
This common widely used paradigm usually reduces definite typical exertional angina pectoris or chest pain due to CAD. However, in randomized trials, coronary stents and bypass surgery have not reduced death or heart attacks as confirmed in the most recent long term trial follow-up.
Moreover, no randomized trial has shown significant reduction in other symptoms commonly attributed to CAD such as atypical chest pain, fatigue, or short windedness. These less direct symptoms are commonly due to a myriad of other factors including lack of exercise (deconditioning), excess weight, sleep deprivation, excess stress, unhealthy food, high blood pressure, and impaired heart muscle pumping unrelated to coronary artery disease, called primary cardiomyopathy. Fatigue and short windedness are also commonly caused by poor heart muscle relaxation between heart beats called stiff heart syndrome or diastolic dysfunction commonly due to alcohol, diabetes, or high blood pressure, rather than coronary artery blockages.
Even though coronary stents and bypass surgery are intended to relieve blockages and improve coronary artery blood flow, no randomized trials have measured coronary blood flow before these procedures to determine if it was sufficiently impaired with sufficiently high morality to benefit from the procedures. Similarly, coronary blood flow was not measured after stents or bypass surgery to see if coronary blood flow was improved or related to improved well-being longevity.
Finally, in the trials of lifestyle, exercise, diet, stents, bypass surgery, or medications treating cholesterol, blood pressure, or diabetes, each of these interventions of medications were tested singly or separately as one intervention, not an integrated comprehensive program incorporating all these steps.
Since no prior trial had done so, the randomized CENTURY Trial tested the benefit of a comprehensive strategy integrating lifestyle, medical treatment of all risk factors and reserving coronary stents or bypass surgery for severely reduced coronary flow capacity by positron emission tomography in chronic CAD. Its design was based on extensive preliminary non-randomized pilot studies over 43 years cumulatively involving over 25,000 patients suggesting reduced death, heart attack, and subsequent invasive procedures after combined lifestyle-medical treatment and coronary stents or bypass surgery guided by cardiac imaging using positron emission tomography (PET). These pilot studies have developed both PET technology and its application now called clinical coronary pathophysiology for achieving beneficial outcomes.
As the first apex test after 54 years of evolving clinical coronary pathophysiology, the randomized CENTURY Trial in chronic CAD demonstrated that comprehensive lifestyle-medical treatment toward all risk factor goals integrated with coronary interventions reserved for severely reduced coronary flow capacity by positron emission tomography (PET imaging) significantly reduced death by 42.7%, death or MI by 37%, and later coronary procedures by 35.1% over 11 years follow-up when compared to standard community care.
These results confirm the clinical value of physiologically guided coronary interventions by coronary flow capacity combined with comprehensive healthy living – pharmacologic risk factor management by frequent supportive patient contact with CENTURY staff compared to standard care. Larger trials of single treatment interventions such as stents, bypass surgery, diet, exercise, or drug treatment separately and without coronary blood flow or integrated comprehensive CV care reported more limited benefits.
The randomized CENTURY Trial and extensive physiological data from large pilot cohorts over long term follow-up demonstrate a potential paradigm changing strategy for managing chronic CAD based on non-invasive, objective coronary flow capacity and subendocardial imaging by quantitative positron emission tomography. This comprehensive, integrated strategy reserves invasive coronary procedures for physiologically severe CAD at high mortality risk or angina pectoris that is reduced by stents or bypass surgery. The vivid, color-coded, easily understood, personalized cardiac PET scans motivate and reassure patients and their physicians for the safety, adherence, and effectiveness of lifestyle and medical treatment toward all risk factor goals for well, active longevity while also reducing non-beneficial invasive coronary procedures now commonly done based on the angiogram alone.
Ongoing development includes (i) simplified clinical reporting format to guide clinical decisions based on the complex PET data for physicians, cardiologists, and radiologists not versed in cardiac PET technology or coronary pathophysiology; (ii) complete automation of PET imaging technology, blood flow measurements, and interpretation integrated with clinical circumstances potentially augmented by AI; (iii) refinement of the quantitative coronary blood flow thresholds for atypical chest pain, short windedness, and fatigue separately from the severe thresholds for which stents and bypass surgery improve longevity.
The work was supported by Al and Celia Weatherhead of Cleveland, their CENTURY Trial funding, the Weatherhead Endowment at UTHealth Houston and charitable donations from many grateful patients. Extraordinary long-term senior UTHealth Houston administration making the work possible include David McPherson, MD; Kevin Dillon, MBA, CPA; Michael Tramonte, MBA, CPA; Melissa Pifko, JD; Sarah Peirce; Jagat Narula, MD, PhD; LaTanya Love, MD; and former UTHealth Houston presidents Giuseppe Colasurdo, MD; David Low, MD, PhD; and Roger Bulger, MD.
Current members of the UTHealth Houston Weatherhead PET Imaging Center for Preventing and Reversing Atherosclerosis who made data collection possible include Nils P. Johnson, MD; Amanda E. Roby, PET,CMNT,RT(N) MBA; Richard Kirkeeide, PhD; Linh Bui, MD; Monica B. Patel, MD; Danai Kitkungvan, MD; Stefano Sdringola, MD; Mary Haynie, RN, MBA; Tracy Pipitoni, RN; Katelyn Garner, RN; Archie Andal, RN; Kelly Sander, PET, CMNT; Lindsey Harmon, PET, CMNT; Li-Wei Chen, PhD; Tung Nguyen; Dejian Lai, PhD; Ruosha Li, PhD; Patricia Mendoza, MBA; Amy Rickman, MBA; Susan Hood; Victor Cuffee Maida; Kenny Castro; Isabel Lopez; Laura Santibanez; An Tran; and Karla Zaragoza.