Treatment Options
The standard treatment of MALS is the release of the celiac artery by open surgical or laparoscopic removal of portions of the median arcuate ligament and ganglionic tissue that surround or completely encase the celiac artery. Regardless of the specific approach, the operation requires meticulous release of the celiac artery by division of muscle fibers from the median arcuate ligament and surgical removal of the overlying lymphatic, ganglionic, and soft tissue. The term “neurolysis” is used to describe the removal of nerve and ganglionic tissue that surrounds the artery in the front, sides, and back. In some patients inflammation and scar tissue is also removed. There are three main types of surgeries to treat MALS, all of which have a role.
Surgical treatments can be done using open, laparoscopic, or endovascular methods. Surgical treatment is aimed to reduce or eliminate pain and improve the quality of life for the patient.
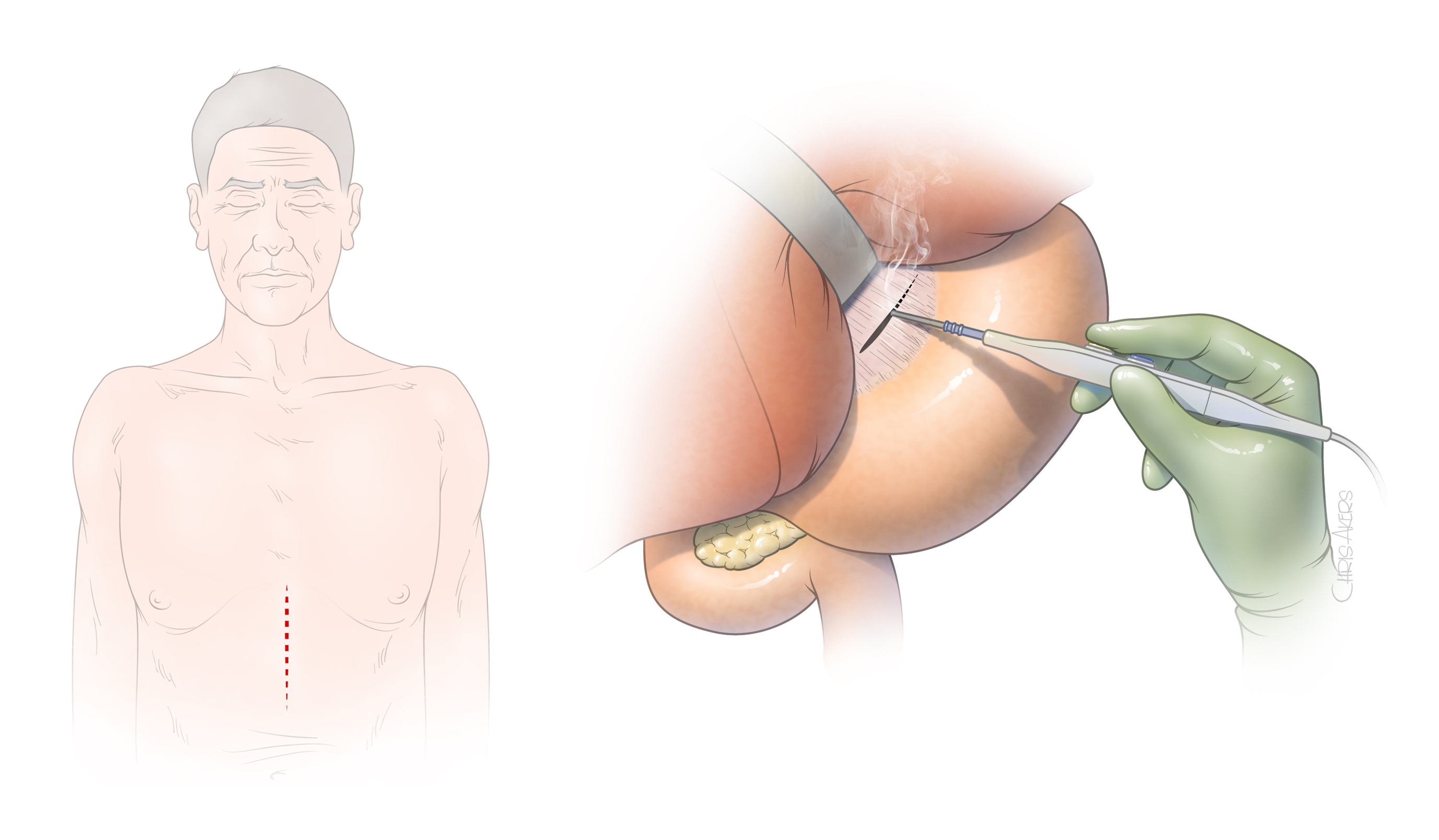
- Figure 3. Open surgical approach is most often done with an incision in the epigastric area. The space between the stomach and the liver is opened to exposure the median arcuate ligament and the celiac artery.
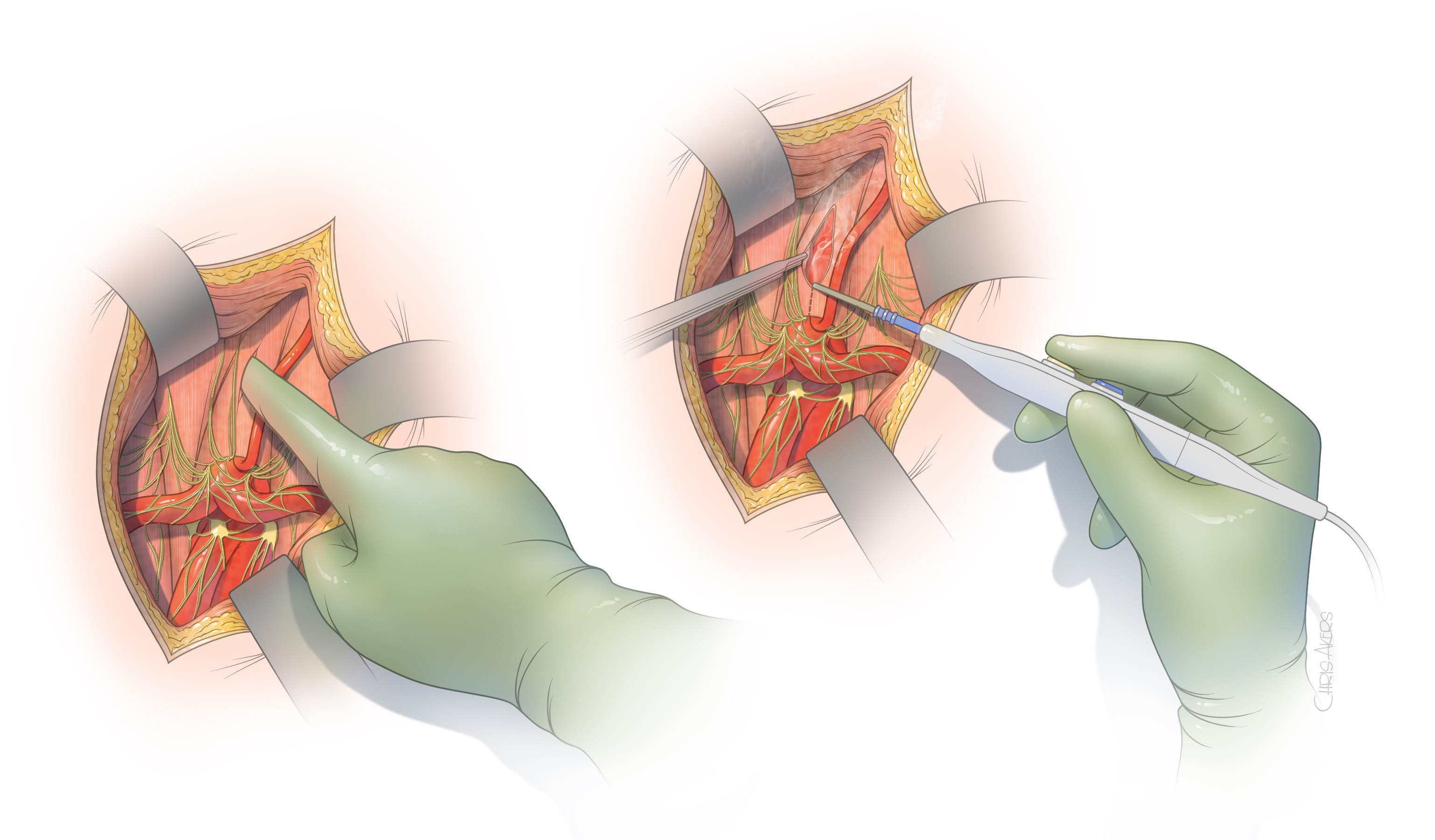
- Figure 4. The surgeon feels the aorta through the muscle of the median arcuate ligament and open the muscle fibers to expose the aorta. Note the nerve and ganglionic tissue surrounds the celiac artery and its branches.
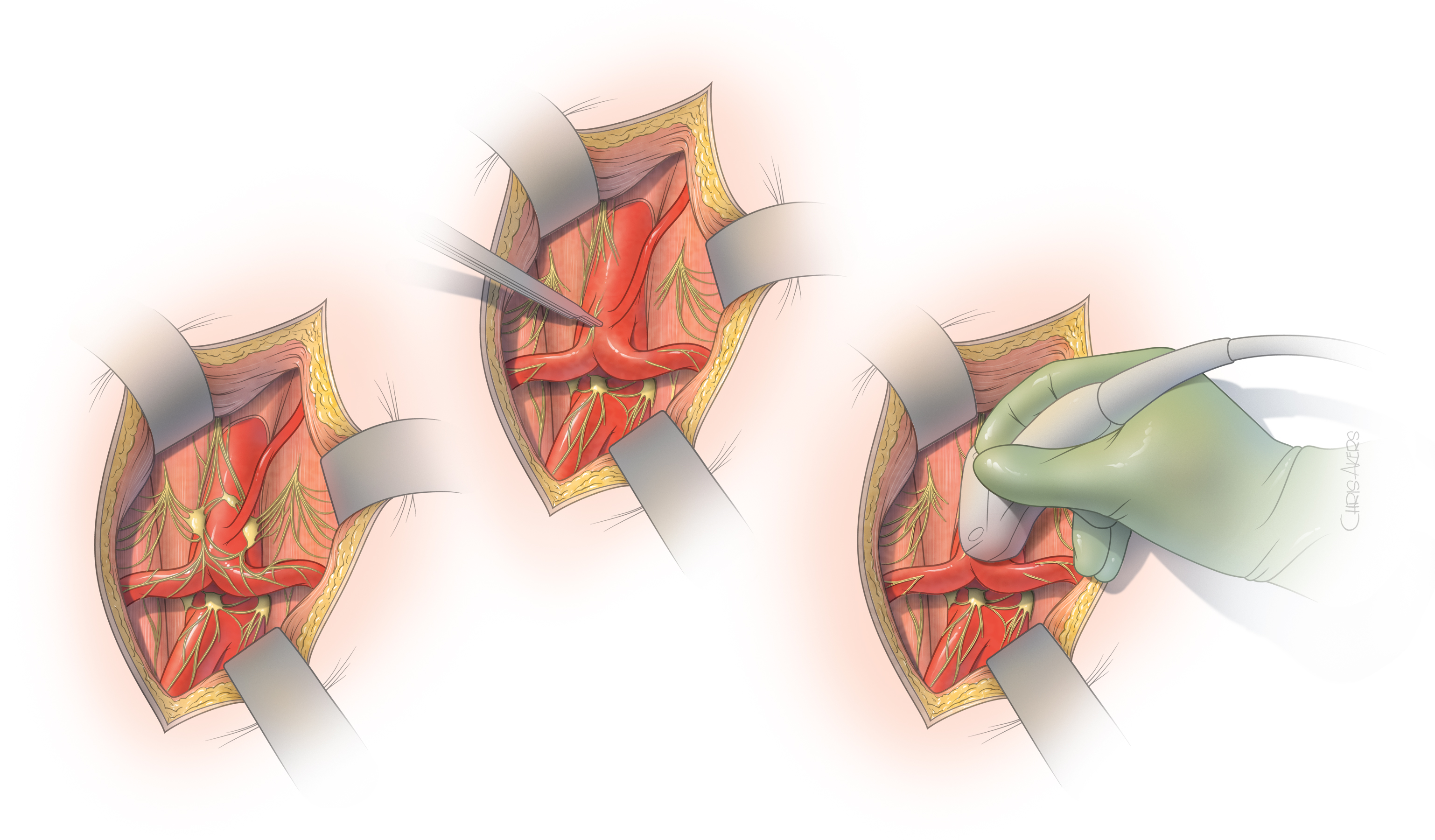
- Figure 5. The median arcuate ligament is completely removed and cleared from the top of the aorta and celiac artery, allowing full expansion of the celiac artery to its normal size. The ganglion and nerve tissue are also removed. Once this is done we typically obtain and ultrasound of the celiac artery during the operation to determine if there is evidence of residual narrowing. Mild or moderate narrowing is typically left alone and can be taken care later if needed using balloon angioplasty or placement of a stent.
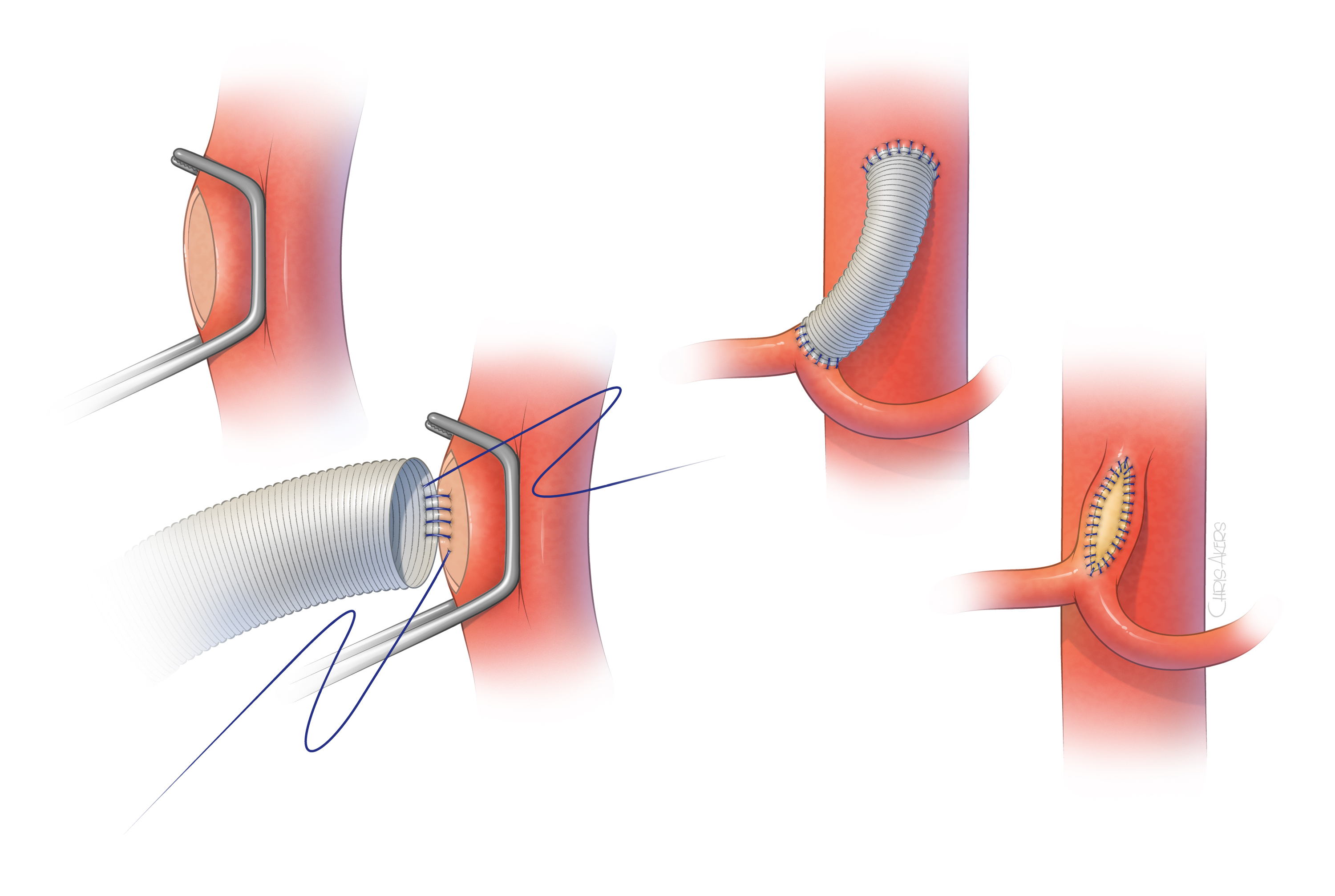
- Figure 6. In some patients the celiac artery may remain occluded or severely narrowed after the surgical release of the median arcuate ligament. In these patients the surgeon may need to perform a short bypass from the aorta to the celiac artery using a prosthetic polyester graft or patch.
Open surgical approach
Open surgical release of the median arcuate ligament is most often done using an incision in the epigastric area (Figure 3). The incision typically extends two-thirds of the distance between the lower end of the breast bone toward the umbilical scar. The surgeon exposes the area between the stomach and liver to visualize the median arcuate ligament. Using a combination of sharp dissection with scissors and cautery, the celiac artery is circumferentially freed from the muscle and ganglionic tissue, which are partially removed (Figure 4). Once the artery is freed, our preference is to obtain an intraoperative duplex arterial ultrasound to document that the artery is not severely narrowed or occluded. In cases of severe narrowing, the artery may be immediately repaired by placement of a small prosthetic patch or graft. The main advantages of the open surgical approach rely on the safety of surgical dissection under direct vision and ability to handle any small tear or areas of bleeding. This approach also allows thorough and complete circumferential release of the artery, including the tissue that lies behind the celiac artery (Figure 5). In addition, any severe narrowing can be immediately repaired (Figure 6). The main disadvantage is the need for the incision and larger exposure.
Laparoscopic approach
Laparoscopic release of the celiac artery requires small holes to introduce the camera and surgical instruments without the larger incision. The surgeon works with camera visualization using scissors and cautery. Although the same steps are performed, the operation has the advantage of smaller incisions and the potential disadvantage of risk of bleeding complications or a less thorough release of the ligament. It is critical that the laparoscopic approach is performed by a surgeon with extensive experience in laparoscopy and familiarity with surgical dissection of the celiac artery. Moreover, if laparoscopy is selected, the procedure needs to be performed in a surgical environment and by a team that is ready to perform the conversion and arterial repair, if needed.
Endovascular approach
An endovascular approach is not recommended as a stand-alone therapy because the muscle and ligament cause persistent compression of the artery, which typically recoils back to its compressed state after the balloon angioplasty. In fact, patients who are treated by angioplasty balloon and stent placement without the prior surgical release of the ligament may experience complete occlusion or fracture of the stent due to the median arcuate ligament compression. Most often, the endovascular approach is used in conjunction with previous laparoscopic or open surgical release to treat residual narrowing of the artery following the surgical release. In these cases, the procedure can be done under a local anesthetic with a small puncture in the groin artery. A catheter is introduced into the celiac artery and the narrowing is dilated with balloon angioplasty. Typically, a stent is also placed.