HIV in Houston
It’s time to end HIV
- In 2018, there were 27,057 people living with HIV in Houston. In 2018, 1,243 people were newly diagnosed with HIV.
- Between 2012 and 2016, the number of persons living with HIV increased by 14%. New HIV diagnoses and HIV-related mortality fluctuated but appear to be stabilizing.
- Rates of new HIV diagnoses and prevalence in both Houston/Harris County and the Houston EMA continue to exceed rates both for Texas and the U.S.
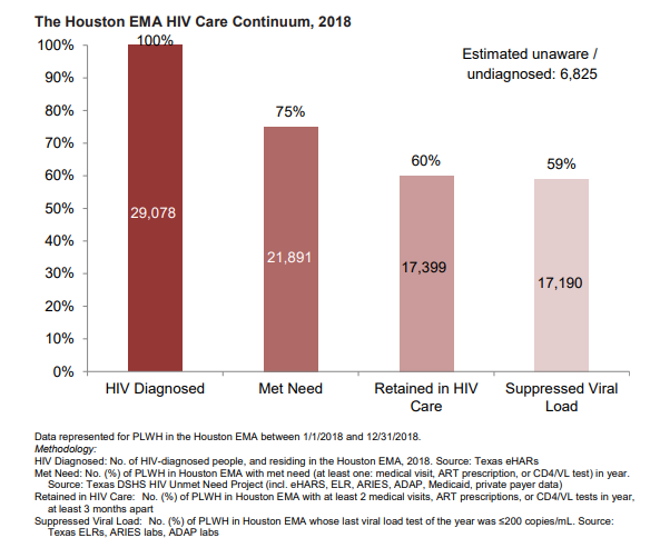
- An estimated 6,825 individuals in the Houston EMA were living with HIV in 2018, but were not diagnosed. Of the 29,078 HIV diagnosed individuals in the Houston EMA in 2018, 75% had met need (at least one: medical visit, ART prescription, or CD4/VL test) in year); 60% were retained in HIV care (at least 2 medical visits, ART prescriptions, or CD4/VL tests in year, at least 3 months apart ); and 59% maintained or reached viral load suppression (≤200 copies/mL).
HIV Prevention
There are now more options than ever before to reduce the risk of acquiring or transmitting HIV. Using medicines to treat HIV, using medicines to prevent HIV, using condoms, having only low-risk sex, only having partners with the same HIV status, and not having sex can all effectively reduce risk. Some options are more effective than others. Combining prevention strategies may be even more effective. But in order for any option to work, it must be used correctly and consistently.
TasP (Treatment as Prevention) and U=U

We now know that medications that treat HIV can also prevent HIV transmission: If you are HIV-positive and take HIV treatment that suppresses your virus to undetectable levels (you have an undetectable viral load), you will not pass HIV to the people you have sex with. In other words, undetectable HIV is sexually untransmittable.
Effective treatment can also prevent HIV transmission to a baby during pregnancy and birth, if the pregnant person maintains an undetectable viral load throughout their pregnancy. Finally, research shows that effective treatment greatly reduces the risk of HIV transmission between people who share drug equipment.
In short, effective HIV treatment not only treats HIV but it can also prevent HIV. Hence the term treatment as prevention (TasP).
PrEP – Pre-Exposure Prophylaxis
PrEP (pre-exposure prophylaxis) is an effective prevention strategy that involves an HIV-negative person who is at risk for HIV taking a certain kind of HIV medication. Once on PrEP, it is important to take the medication as prescribed and to see a doctor or nurse every three months to get tested for HIV and other STIs and to check for side effects.