A Collaborative Approach Offers Patients a Less Invasive Alternative for Surgical Excision of Pituitary Tumors
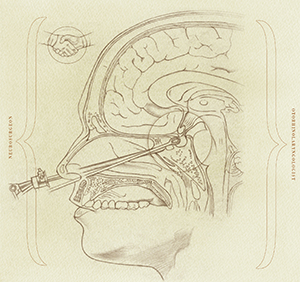
Surgery is the primary treatment for pituitary tumors and until the last decade, neurosurgeons favored the traditional microscopic sublabial transseptal approach – an incision under the lip, use of a retractor to push away nasal tissue and placement of a microscope to view the tumor, followed by excision, suction and removal. Today, many centers – including Memorial Hermann-Texas Medical Center – have adopted a collaborative endoscopic transnasal approach in which an otorhinolaryngologist and neurosurgeon work together to locate and excise the tumor. Fifty-four-year-old Lewis Tyra is one of many patients who have benefited from the less invasive approach made possible by the collaboration of Arthur L. Day, MD, an internationally renowned neurosurgeon with expertise in cerebrovascular and skull base neurosurgery, and Samer Fakhri, MD, FACS, FRCS(C), an internationally recognized rhinologist with expertise in minimally invasive, image-guided skull base surgery.
Tyra suffered progressive, undiagnosed loss of peripheral vision in his right eye over a period of about six months before an ophthalmologist ordered an MRI that revealed a pituitary tumor. His wife Patsy Tyra sat down at their computer and began an Internet search for doctors.
“Dr. Day’s name kept popping up, so we called the Mischer Neuroscience Institute (MNI) and his nurse asked us to have the MRI results sent over,” Tyra says. Based on his longstanding interest in the treatment of pituitary tumors, Dr. Day spearheaded the opening of MNI’s Pituitary Tumor and Vision Change Clinic in 2011 to ensure early and precise diagnosis of pituitary and other parasellar tumors using an integrative approach.
“The idea of using the endoscope rather the microscope for removal of pituitary and other parasellar tumors came from the ENT service,” says Dr. Day, who is a professor and vice chair and director of clinical education in the Vivian L. Smith Department of Neurosurgery at The University of Texas Health Science Center at Houston (UTHealth) Medical School. “Neurosurgeons have been using the endoscope for only about the last 10 years. I wanted MNI’s pituitary program to have the latest and greatest technique and technology. The collaboration with otorhinolaryngology was a natural fit.”
Otolaryngologists began using the endoscope for sinus surgery in the 1980s because it offered the advantage of a close-up view of a suspect area in a minimally invasive way. “Once we got comfortable using the endoscope for sinus surgery, we expanded our horizons and pushed the envelope, using the technology to access the orbit, skull base and beyond, and to remove nasal tumors,” says Dr. Fakhri, who is an associate professor and residency program director in the department of Otorhinolaryngology-Head and Neck Surgery at McGovern Medical School. “Eventually, it occurred to us that neurosurgeons could use the same transnasal approach to access and manage skull base pathology. Otorhinolaryngology had a successful track record with the approach, so why not collaborate with neurosurgery to improve the patient experience?”
The primary advantage of the endoscope over the microscope is better visualization of the tumor and tumor boundaries, and most importantly, the ability to see around corners. During the microscopic procedure, the microscope rests outside the patient’s nose, and it is only possible to visualize what is directly in the view of the microscope.
“The microscope magnifies the tumor but can visualize only in a straight line,” Dr. Fakhri says. “It’s very much like looking through a keyhole – all you can see is straight ahead and a bit of the horizon. But if you insert a telescope through the keyhole, you have a panoramic view in all directions that allows you to do one very important thing – visualize a tumor hiding behind corners and bony ledges.”
Lewis Tyra’s surgery was scheduled for March 6, 2012. “We view the surgery as a joint effort,” Dr. Fakhri says. “Using an otorhinolaryngologist’s knowledge of the nasal structures, paranasal sinuses and skull base, we approach the tumor in the least invasive way, opening the area to expose it and then opening the lining of the brain. While I’m guiding the endoscope, Dr. Day removes the tumor and then I close the skull base endoscopically.”
Image guidance, a GPS-like tracking device, was used throughout the procedure to guide the dissection and identify landmarks. In addition, navigation CT-MR fusion protocols allowed the surgeons to switch back and forth between views of bone and soft tissue until the tumor was completely removed.
From the patient perspective, the surgery is less invasive and less destructive of surrounding tissue. Tyra regained his vision immediately following the surgery.
“When you hear the words brain and tumor in the same sentence, you think this can’t be good. I was halfway convinced I was not going to see again,” Tyra says. “When I woke up in recovery, I could read the clock on the wall, even without my glasses. I remember that it was 6:45 p.m. I felt like I could have gotten up out of the recovery room and gone home. By the next morning, I literally could not tell that I had had a surgery.”
The case was very straightforward, Dr. Day says. “Lewis was in the hospital a day or two and felt better immediately. He had complete preservation of pituitary function, and a follow-up MRI showed complete removal of the tumor.”
 “The idea of collaborative pituitary surgery is to pair the same otorhinolaryngologist and neurosurgeon,” Dr. Fakhri says. “When you perform the procedure together over and over again, you learn to work together very smoothly.”
“The idea of collaborative pituitary surgery is to pair the same otorhinolaryngologist and neurosurgeon,” Dr. Fakhri says. “When you perform the procedure together over and over again, you learn to work together very smoothly.”
One disadvantage of the traditional endoscopic approach is the two-dimensional image it provides versus the 3D view of the microscope. Recently surgeons at Memorial Hermann-TMC’s have trialed 3D endoscopy technology, which serves to eliminate that disadvantage.
“We are driven in this day and age by evidence, outcomes and cost containment,” Dr. Fakhri says. “So we always ask the question: Does it really result in better outcomes and better quality of life? A number of publications comparing the two approaches indicate that the endoscopic approach is less costly than the microscopic approach in terms of total expenditure on care. It also has better preservation of nasal function. Data on completeness of tumor removal and quality of life after surgery are conflicting, but it is safe to say that both techniques are roughly equal in that regard.”