Collaboration Across Specialties Leads to a Good Outcome for Lolita Hernandez
 After two hospitalizations in 2021 – one in February for dehydration and the second in September for acute colitis – Lolita Hernandez went to her primary care physician for a checkup, complaining of joint, muscle, and bone discomfort. When her blood test results showed hypercalcemia, her family physician referred her to Edward Nicklas, MD, an endocrinologist with Memorial Hermann Medical Group, who first saw her in December 2021.
After two hospitalizations in 2021 – one in February for dehydration and the second in September for acute colitis – Lolita Hernandez went to her primary care physician for a checkup, complaining of joint, muscle, and bone discomfort. When her blood test results showed hypercalcemia, her family physician referred her to Edward Nicklas, MD, an endocrinologist with Memorial Hermann Medical Group, who first saw her in December 2021.
“It came out of the blue, and I had been having symptoms for about a year,” says Hernandez, now 59. “I noticed that my tongue was larger than normal, and my knuckles seemed huge.”
“The referral was for hypercalcemia, but she had some signs of acromegaly, with increased skin folds, a large tongue and hands, and increased space between her teeth,” Dr. Nicklas says. “We ordered an insulin-like growth factor 1 test (IGF-1), and the results showed high production of growth hormone, which is made by cells in the pituitary gland and is involved in many cell processes in the body, including growth during childhood.”
Hernandez also had hyperthyroidism and a thyroid nodule. Dr. Nicklas did a fine-needle aspiration biopsy of the nodule, with an indeterminate pathology result. Given the possibility of increased thyroid cancer risk in people with acromegaly, he referred his patient to Ibrahim “Trey” Alava III, MD, associate professor and vice chair for quality and patient safety in the Department of Otorhinolaryngology at McGovern Medical School at UTHealth Houston and chief of otolaryngology surgery at Lyndon B. Johnson Hospital, part of Harris Health System.
“When I saw Ms. Hernandez, she had a palpable thyroid nodule, and an ultrasound showed more than one nodule,” Dr. Alava says. “I reviewed her family history, considered the ultrasound results and biopsy report, and told her I thought the best approach would be a thyroidectomy. That would cure her overactive thyroid and it would also provide a diagnosis for her indeterminate nodule, which turned out to be papillary thyroid cancer.” He removed her thyroid in April 2022.
The results of the lab tests ordered by Dr. Nicklas also suggested an autonomously overactive parathyroid gland, which he thought was contributing to her hypercalcemia. During the thyroid surgery, Dr. Alava found an enlarged parathyroid gland and removed it.
As part of his initial testing, Dr. Nicklas also ordered an MRI of the pituitary in the knowledge that too much growth hormone usually is related to a pituitary adenoma. Upon viewing a large adenoma on her imaging results, he referred her to Spiros Blackburn, MD, associate professor in the Vivian L. Smith Department of Neurosurgery and director of the Pituitary Tumor Center at UTHealth Houston Neurosciences, and William Yao, MD, associate professor of otorhinolaryngology and director of the otolaryngology residency program. The two surgeons work together to remove pituitary tumors, operating in tandem using a transsphenoidal endoscopic approach to improve outcomes and minimize recovery time.
“Given the location of the tumor, how tightly it was adhered to the right internal carotid artery, and the significant risk of potential carotid injury, we decided it was safer to leave some tumor,” Dr. Yao says. “This is why complex patients require a multidisciplinary approach. Dr. Nicklas is medically managing Ms. Hernandez to ensure that her symptoms remain controlled.”
In February 2023, Hernandez’s MRI result showed that the tumor was stable. “She has a mixed tumor, which is very rare in the literature – a mixture of gangliocytoma and pituitary adenoma. She has had a decrease in her IGF-1 level with the tumor removal and with her monthly lanreotide injection, which blocks the release of growth hormone,” Dr. Nicklas says. “Our goal is an IGF-1 level in the normal range to improve symptoms and decrease the potential effects of excess growth hormone in the body, such as an enlarged heart. Ms. Hernandez has had significant improvement in symptoms with her treatments.”
“It often happens that patients with rare disorders like Ms. Hernandez see different doctors who provide care for bits and pieces of the condition in silos,” Dr. Alava says. “Our clinically integrated approach allowed us to provide her care as a team, which improves outcomes.”
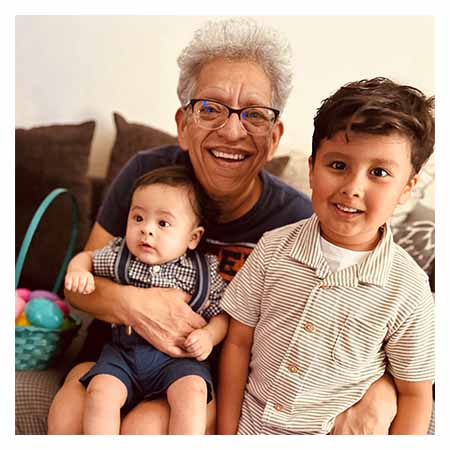
Dr. Nicklas sees Hernandez monthly in his clinic. “In cases of hypercalcemia, we usually think of two main causes – primary hyperparathyroidism and cancer – but it’s important to also consider the unusual causes,” he says. “We made a presumptive clinical diagnosis of multiple endocrine neoplasia Type 1, which typically includes pituitary, parathyroid, and pancreas abnormalities. She hasn’t had signs of pancreas abnormality, but we will monitor this over time. Ms. Hernandez has been through quite a lot and has had to endure multiple medical procedures and follow-up. I’m amazed at her positive attitude and calmness through all of this. She brightens our clinic every time we see her.”
“I thank God and the doctors because they did a tremendous job,” she says. “I feel much better. I can honestly say I felt the difference when they let me out of bed three or four hours after surgery. The doctors all did a great job. They really did.”