New Clinical Learning Guidelines Transform How Medical Residency Programs Prepare Future Physicians
In January 2014, the Accreditation Council for Graduate Medical Education (ACGME) released updated guidelines for graduate medical education in training programs across the United States. The new Pathways to Excellence framework is the latest development in the national rollout of the Clinical Learning Environment Review (CLER) program, initiated in 2012 to ensure excellent learning environments for more than 117,000 residents and fellows at teaching hospitals and academic medical centers.
The CLER program, an ongoing initiative to assess the learning environment at each ACGME-accredited institution, adds an additional layer of checks and balances as residency and fellowship programs transition to the Next Accreditation System (NAS).
 “The ACGME has identified skills critical to independent practice and established milestones to serve as guideposts along the way as residents and fellows progress through their programs,” says Ronda Alexander, MD, an assistant professor and residency program director in the Department of Otorhinolaryngology-Head and Neck Surgery at UTHealth Medical School. “Instead of locking down the process and wondering about the product, we’ve unlocked the processes and defined the products we want.”
“The ACGME has identified skills critical to independent practice and established milestones to serve as guideposts along the way as residents and fellows progress through their programs,” says Ronda Alexander, MD, an assistant professor and residency program director in the Department of Otorhinolaryngology-Head and Neck Surgery at UTHealth Medical School. “Instead of locking down the process and wondering about the product, we’ve unlocked the processes and defined the products we want.”
Otorhinolaryngology, like other specialty groups, now uses outcomes-based milestones as a framework for benchmarking resident performance within the six ACGME core competencies: medical knowledge, patient care, professionalism, interpersonal communication, personal practice improvement and system-based practice. “In residency you want to see a new doctor progress from being able to collect data to the correct interpretation of that data, to knowing what to do with the data and being able to safely complete a procedure or treatment plan in all of the disciplines within our specialty. The milestones are developmental stages that can be demonstrated progressively by residents and fellows from the beginning of their education through graduation,” says Dr. Alexander, who directs the Texas Voice Performance Institute. “Under the previous system, evaluations were more subjective and based on whether a faculty member believed the resident was at the appropriate level for his or her year of training. Now we have clearly defined skills and behaviors that residents can accomplish in any year at their own pace.”
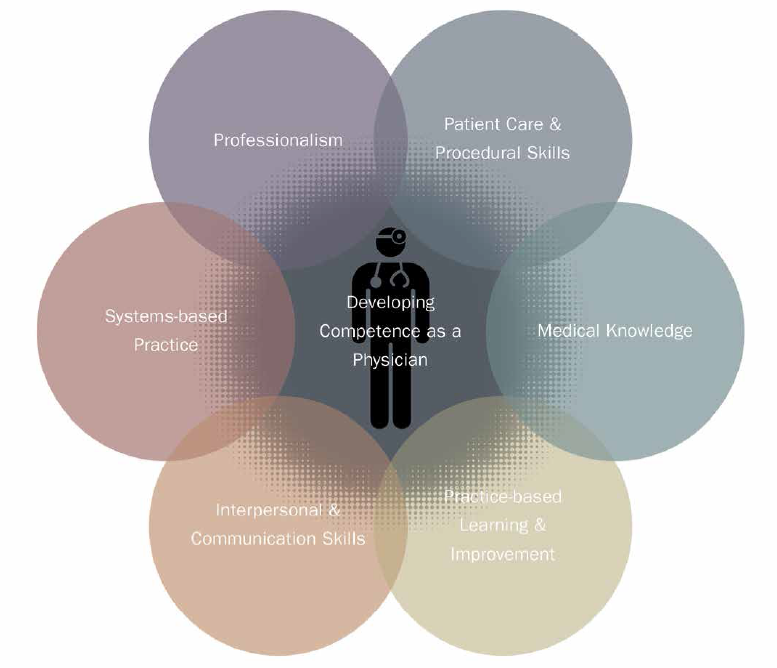
ACGME has identified 6 core competencies for all physicians and measures accomplishment through outcomes-based tracking of milestones that gauge resident performance.
Third-year resident Jaecel Shah, MD, believes the new system helps individualize learning for the department of Otorhinolaryngology-Head and Neck Surgery’s 10 residents. “In addition to being evaluated by the faculty, we do periodic self-assessments to evaluate domains we should work harder to develop,” Dr. Shah says. “The new system is designed to ensure that we get the most complete training possible with a minimal number of potholes – in other words, it maximizes our steps forward.”
The NAS structure also allows faculty to identify deficiencies sooner rather than later. “We can identify learners who are struggling to achieve their milestones earlier and intervene with the appropriate educational tools,” Dr. Alexander says. “Our transition to the new system is a continuous prospective process. It’s an area in which we’re free to innovate as we revise our processes to align with the ACGME’s goals.” The new CLER Pathways to Excellence – the next step forward – was summarized in a paper published in the Jan. 27, 2014, online edition of the New England Journal of Medicine and announced to healthcare leaders at a policy forum in Washington, D.C. It represents a roadmap for the approximately 700 accredited institutions and their 9,000 residency and fellowship programs across the country to improve resident and fellow physicians’ skills in addressing issues of patient safety and healthcare quality as an essential component of modern medical practice.
“We’re reshaping the clinical environments in which future physicians learn to provide quality patient care and at the same time respond to rapid changes in the healthcare delivery system,” Dr. Alexander says. “New physicians are learning to work in complicated and unpredictable settings. They’re benefiting from more defined expectations, explicit feedback from faculty and earlier identification of areas in which they need additional support.”