Rapid Response and Multidisciplinary Teamwork Save a Young Man’s Life
A gunshot wound to the face – a random act of violence in Beaumont, Texas – forever changed the life of 21-year-old Adair Stephens. The shooting occurred late in the afternoon on a Saturday in September 2013.
After being rushed to the emergency center at Baptist Beaumont Hospital, Stephens was transported by Memorial Hermann Life Flight® to the Texas Trauma Institute at Memorial Hermann-Texas Medical Center, where the Level I trauma team stabilized him. He was taken to the OR by ophthalmologist Nan Wang, MD, PhD, for treatment of an open globe laceration to the left eye caused by the bullet. Ophthalmic plastic and reconstructive surgeon Margaret E. Phillips, MD, was called into surgery to explore the orbit on the right side for a suspected foreign object. Also on hand was otorhinolaryngologist Ibrahim “Trey” Alava III, MD, who assessed Stephens and scheduled him for surgery the following Monday to clean out the mid-face and begin the reconstructive process.
“The bullet entered Adair’s right lower cheek, went through the mid-face and roof of the mouth, exploded his left eye socket and lodged in the soft tissue above the eye,” says Dr. Alava, an assistant professor in the Department of Otorhinolaryngology-Head and Neck Surgery at UTHealth Medical School.
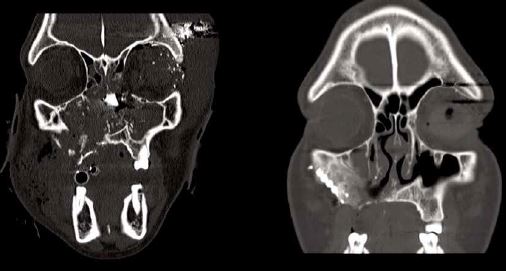
The CT image on the left was made immediately following the patient’s injury, and shows shattering of the facial skeleton with visible residual bone fragments. On the right, a postoperative scan shows restoration of the normal and symmetric bony contours of the maxillofacial skeleton.
During his two-month hospitalization, Stephens underwent five additional surgeries. Dr. Alava performed a tracheostomy to provide an airway and remove secretions from his lungs. He stabilized his upper face by wiring it to the jaw to keep the mid-face immobile, allowing for minimal movement and maximal healing. To decrease the risk of infection he washed out the area and also removed a portion of the bullet that had lodged in his sphenoid sinus. During his hospitalization, Dr. Phillips removed his left eye.
“Ophthalmology followed Adair closely over many weeks,” says Dr. Phillips, who is chief of ophthalmic plastic and reconstructive surgery at the Robert Cizik Eye Clinic and a clinical assistant professor at UTHealth Medical School. “He maintained normal vision and movement in the right eye, but we couldn’t save the left eye due to the severity of the open globe injury. After he recovered from the enucleation of the left eye, a prosthesis was made to duplicate his natural eye.”
In a final reconstructive surgery, Dr. Alava performed an open reduction and internal fixation of the mid-face with titanium plates, and rotated a palate flap to close the hole created by the bullet between the sinus and oral cavity. He closed the tracheostomy before Stephens was discharged.
Stephens’ mother, Cassandra Stephens, remained by her son’s side during his entire hospitalization. He was discharged in late October, nearly two months after his admission. “We knew Adair would need some revisions later on, including sinus surgery to recreate a sinus cavity on the right side and scar revisions from the bullet wounds and the tracheostomy,” says Dr. Alava, who has a special interest in reconstructive surgery following trauma. “But I was very pleased with his condition when he was discharged. He had been home about a day and a half when his mother called and told us he had spit up some blood. I’d done multiple surgeries behind the nose so the presence of a small blood clot might be expected.” Stephens took her son back to the emergency center at Baptist Beaumont Hospital. After talking with an emergency physician in Beaumont, Dr. Alava’s medical assistant Lisa Martinez-Ward, became concerned and alerted him. “Based on his vital signs, I immediately thought Adair had developed a lingual artery aneurysm and called for a Life Flight transport back to Houston,” Dr. Alava says. “Lisa was very astute in recognizing a life-and-death situation.” Upon his arrival, Stephens was admitted to the Memorial Hermann Mischer Neuroscience Institute at the Texas Medical Center, where neurosurgeon and endovascular intensivist P. Roc Chen, MD, embolized the lingual artery aneurysm, saving Adair’s life. He was cared for in the Neurotrauma ICU for the four days, and then admitted to the otolaryngology service for observation.
“We’re very fortunate to be able to offer our patients access to a top-notch team of physicians from many disciplines,” Dr. Alava says. “In this case, ophthalmology, otorhinolaryngology and neurosurgery worked together to save Adair’s life.”
Cassandra Stephens is grateful for the care her son received. “They all did an excellent job,” she says. “If it hadn’t been for their skill and God’s grace, Adair wouldn’t be here with me.”