Inflammatory Bowel Disease
Offering Individualized Care and Treatment
UT Physicians Colon and Rectal Surgery team works closely with you to create a highly individualized treatment plan based on the type and severity of the symptoms. Treatment options may include dietary changes, medications, and, in some cases, surgery. If surgery is necessary, we are experts in laparoscopic procedures to cure or relieve IBD symptoms. The following procedures performed by our team are just three examples of our expertise:
- Laparoscopic Small Bowel Surgery – A small bowel resection is a surgery to remove a diseased section of the small intestine. The laparoscopic technique involves small incisions and faster recovery. In this procedure, the diseased section of the small intestine is stapled and removed; then, the two bowel ends are reattached using staples.
- Laparoscopic J-Pouch Surgery – This procedure can often “cure” those patients with ulcerative colitis as well as eliminate their risk of colorectal cancer. The J-pouch procedure is the common name used for the operation that removes the entire colon and rectum and replaces the rectum with a neorectum, or new rectum, a pouch made from the last portion of the small intestine and connected to the anus.
- Laparoscopic Restorative Proctocolectomy – Restorative proctocolectomy is a standard treatment for advanced IBD. UT Physicians Colon and Rectal Surgeons typically perform this technique via a laparoscopic or minimally invasive approach, while most surgeons often use an open approach, requiring a much larger incision.
Crohn’s Disease Vs. Ulcerative Colitis
Crohn’s disease and ulcerative colitis are so similar they are often mistaken. Both are chronic inflammation in the digestive tract lining, but Crohn’s disease can spread deep into the layers of affected tissues. In contrast, ulcerative colitis usually affects only the innermost lining of the colon and rectum.
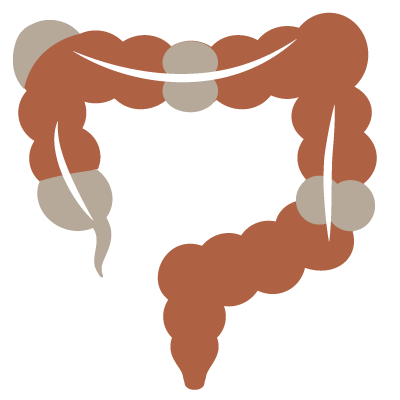
Understanding Crohn’s Disease
Crohn’s disease may affect the GI tract anywhere from the mouth to the anus. However, the ileocecal region, the last part of the small bowel with the first part of the colon, is most commonly affected. Treated primarily with medicine, surgery is typically needed at some point during Crohn’s disease. A severe flare of Crohn’s may require hospitalization and emergency surgery. Crohn’s disease in the colon carries an increased risk for colon cancer.
Understanding Ulcerative Colitis
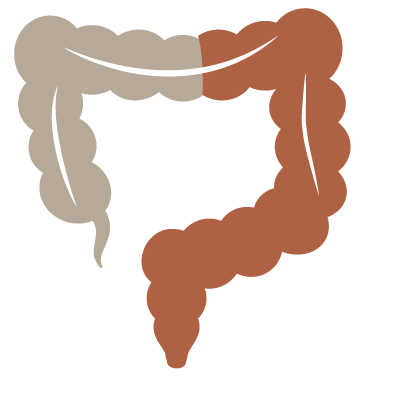 Ulcerative colitis involves the rectum and some or all of the colon. A severe flare of ulcerative colitis may require hospitalization, and if the disease cannot be controlled medically, surgery is necessary. Ulcerative colitis is curable with surgery by removing the entire colon and rectum. In most cases, a permanent ileostomy can be prevented by constructing a pouch made out of small bowel and connected to the anus, called a J-Pouch. Ulcerative colitis does carry an increased risk of colon cancer. Sometimes surgery is recommended based on the duration of the disease or abnormal changes in the colon’s lining called dysplasia that make the risk of colon cancer too high to continue to follow the patient’s medical treatment.
Ulcerative colitis involves the rectum and some or all of the colon. A severe flare of ulcerative colitis may require hospitalization, and if the disease cannot be controlled medically, surgery is necessary. Ulcerative colitis is curable with surgery by removing the entire colon and rectum. In most cases, a permanent ileostomy can be prevented by constructing a pouch made out of small bowel and connected to the anus, called a J-Pouch. Ulcerative colitis does carry an increased risk of colon cancer. Sometimes surgery is recommended based on the duration of the disease or abnormal changes in the colon’s lining called dysplasia that make the risk of colon cancer too high to continue to follow the patient’s medical treatment.
Let our Team Diagnose Your Issue
Symptoms that Crohn’s disease and ulcerative colitis may share include abdominal pain, fever, bleeding, and diarrhea. With Crohn’s disease, some people develop inflammation in their anal region, which may be mistaken for other diseases. Laboratory tests, endoscopic procedures, and radiology tests are used to diagnose IBD. Your colorectal specialist can help you determine the best course of action for diagnosis and treatment.
Crohn’s and Colitis Foundation of America (CCFA)
UT Physicians Colon and Rectal and Gastroenterology Team continues to partner with the CCFA to raise money and increase awareness of IBD-related diseases. The first step to creating more awareness is community involvement. Please help us “take steps” toward a cure and get involved. Visit CCFA.org for more information on upcoming events.